|
 |
- Search
| Arch Hand Microsurg > Volume 27(4); 2022 > Article |
|
Abstract
Although several studies exist on the simple volume filling of soft tissue defects in lower extremity reconstruction, few reports have described functional reconstruction. In this study, a 52-year-old male patient, after a forklift accident, developed soft tissue defects of the all the right dorsiflexors. The patient underwent surgery with a chimeric anterolateral thigh free flap (cALT-FF), in which 18×8 cm2 fasciocutaneous flaps were harvested, including a 6×9 cm2 vastus lateralis muscle flap in a chimeric pattern. The functionality of the lower extremities was evaluated in terms of the active ankle-dorsiflexion range of motion and the Stanmore system after 15 months, and the result was good. In this study, we focused on functional reconstruction following the use of cALT-FF in a patient with defects of all the dorsiflexor muscles, which play an important functional role in gait.
With the remarkable developments in reconstructive microsurgery, reconstruction of lower limb damage is not only a simple way to fill the deficiency site but also an advanced functional reconstruction that aims at the functional restoration of the deficiency site.
The primary goal of functional reconstruction of the lower extremities is allowing the patient to walk properly without pain. Dorsiflexion is an important function necessary for walking, and the anterior compartment muscles of the lower extremities are responsible for it [1,2]. If this function is damaged, foot drop and walking disorders may arise [1,2]. Several studies have reported the simple volume filling of soft tissue defects in lower extremity reconstruction. However, functional reconstruction of the lower extremity is challenging and has rarely been reported [3].
Recently, chimeric flaps have gained popularity because of their unique ability to restore composite defects of the lower extremities while maintaining economic tissue use and low donor-site morbidity [4]. Therefore, we aimed to introduce a successful functional reconstruction case using a chimeric anterolateral thigh free flap (cALT-FF) for repairing a total defect of the anterior compartment muscles and soft tissue in the lower extremity. We focused on the functional reconstruction. Although the cALT-FF already has been used to reconstruct for lower extremity defects, reports focused on functional reconstruction for lower extremity defects are limited.
This study was conducted in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained for publication of this case report and accompanying images.
A 52-year-old male patient had a right distal tibia and fibula open fracture (Gustilo IIIC [5]) with a crushing injury to the right leg due to a forklift accident. After the initial orthopedic treatment, the patient presented with a soft tissue defect with metal plate exposure and a muscle defect in the entire anterior compartment, including the dorsiflexors tibialis anterior (TA), extensor halluces longus (EHL), extensor digitorum longus (EDL), and fibularis tertius (FT). As confirmed in physical examination, he was unable to dorsiflex and had a foot drop in the right ankle due to muscle injury in the anterior compartment of the leg.
Computed tomography images immediately after trauma revealed a 3.5-cm long muscle defect in the anterior compartment of the right distal leg (Fig. 1). Computed tomography angiography results revealed normal vascularity of the lower extremities.
Since the patient had both muscle and soft tissue defects, we used a chimeric flap with multiple components. Furthermore, we decided to reconstruct the muscle and soft tissue defects with a contralateral cALT-FF. After the debridement of the soft tissues and muscles, the length of the muscle defect measured 6 cm (Fig. 2C). We harvested a flap consisting of an 18×8 cm2-sized fasciocutaneous component and a 6×9 cm2-sized vastus lateralis (VL) muscle component in a chimeric pattern (Fig. 2A, 2B, 2D). These two components were supplied by the descending branch of the lateral circumflex femoral artery (LCFA). The fasciocutaneous component had two perforators, and the muscle component had one perforator. The length of the perforators of the fasciocutaneous component was 18 cm and 8 cm long from the pedicle, and the length of the perforator of the muscle component was 15 cm from the pedicle. The distal perforator of the fasciocutaneous component was connected to the perforator of the muscle component.
The perforating branch of the LCFA of the flap was anastomosed end-to-end to the right anterior tibial artery. The accompanying vein of the flap was then anastomosed end-to-end with a vena comitans of the right anterior tibial artery. Additionally, a split skin graft was performed to cover the subcutaneous area of the flap and the donor area remaining after primary repair. A short leg splint was applied at the end of the surgery, and a fluffy gauze dressing was placed.
The surgical scheme is presented in Fig. 3. There were no acute complications such as loss or necrosis in the flap. After 2 months, the flap remained stable. After 3 months, functional defects, such as dorsiflexion and foot drop, improved.
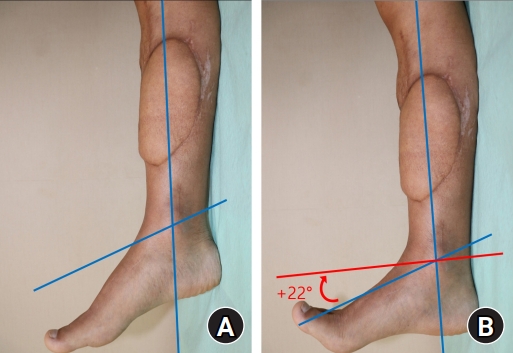
The follow-up period was 15 months. Photographs were taken when the patient could achieve the maximum active dorsiflexion in the supine position and extended knee position (0°), and the angle of the ankle-dorsiflexion range of motion (ROM) in the image was measured. The axis was centered over the medial malleolus, and the arms were aligned with the tibial shaft and head of the fifth metatarsal [6]. After 15 months, he could dorsiflex up to 0° (Fig. 4), and the angle improved by 22° compared to –22° before the surgery. Moreover, the patient was able to ambulate without an orthosis. Applying the Stanmore system to assess the final post-reconstructive ankle function, the patient’s total score was 86, indicating a “good” result [6].
Trauma to the entire anterior lower leg muscle group causes functional defects such as foot drop or gait abnormality [1,2]. The restoration of these lower extremity functions is challenging. In the present case, the damaged area was located in the anterior compartment, and the patient had a foot drop. With a total deficit of 6.0 cm in all the dorsiflexors, the primary repair was impossible due to the large size of muscle and soft tissue defect. Volume coverage and functional reconstruction were required. Although cALT-FF has already been widely used in lower extremity reconstruction in various papers including Kim et al. [7], these focused on structural reconstruction. Unlike previous cases, the difference in this case is to focus on functional reconstruction for lower extremity defects. To the best of our knowledge, the case of the cALT-FF focused on functional reconstruction for lower extremity has not been previously reported.
The concept of the chimeric flap was introduced by Hallock in 1991 [8]. It was defined as a flap that “consists of multiple otherwise independent flaps that each have an independent vascular supply, with all pedicles linked to a common source vessel” [8]. Chimeric flaps are suitable for complex and large defects because they can provide a large amount of soft tissue and multiple components that individual flaps cannot offer [8]. In particular, cALT-FF are widely used due to low donor-site morbidity. Generally, for the cALT-FF, the VL muscle is harvested simultaneously with a skin paddle [9]. The VL muscle lies in the same anatomical territory as the ALT muscle. Furthermore, it offers an advantage in that the surgeon can determine the three-dimensional form of the flap, which is not dependent on the shape of the body [10]. In our case, the VL was also used as a muscle component of the chimeric flap, and there was no significant functional morbidity at the donor site.
The anterior compartment comprises four muscles: EDL, EHL, FT, and TA. They are called dorsiflexors as they have their origin at specific points on the tibia or fibula and insertion in certain areas of the foot [1]. Consequently, contraction of these muscles shortens the body of the muscle and causes the dorsum of the foot to be pulled toward the leg [1]. This movement is known as dorsiflexion. The normal dorsiflexion angle is 0° to 30° [2]. If the dorsiflexor muscles are weakened, foot drop or foot deformation occurs, causing walking disorders [1].
The Stanmore system used in this case for postoperative functional assessment of the lower limb was originally devised to evaluate the functional results of postoperative posterior tibial tendon transfer or functional muscle transfer [6]. Since there is no accurate standard evaluation tool for evaluating function after muscle replacement, we used the Stanmore system to evaluate ankle function. The categories of the Stanmore system are pain, need for an orthosis, ability to wear normal shoes, functional outcome, muscle power, degree of active ROM, and foot posture [6]. The patients’ scores were 10 out of 15, 15 out of 15, 5 out of 5, 6 out of 10, 25 out of 25, 20 out of 25, and 5 out of 5, respectively. The total score was 86, indicating a “good” result.
In this study, the patient could not dorsiflex immediately after the accident. After reconstruction with cALT-FF, he was able to dorsiflex up to 0°. Moreover, the result of the functional evaluation according to the Stanmore system was “good.” Therefore, we considered this to be a successful case.
This study had several limitations. First, we did not use a goniometer, which is a tool to measure ankle-dorsiflexion ROM, and instead measured the angle using an image obtained through photography, which may have led to few errors in this process. Second, ankle-dorsiflexion ROM was not evaluated before the accident, and it is difficult to determine the extent of restoration. Third, only passive ROM was measured; active ROM was not measured.
With breakthroughs in reconstructive microsurgery, reconstructive surgeons should consider not only aesthetic reconstruction but also functional reconstruction. In this study, we focused on functional reconstruction after cALT-FF for defects in the anterior compartment of the lower leg, which comprises the dorsiflexors. In conclusion, from a perspective of functional reconstruction, cALT-FF could be considered as an option for total defects in the anterior compartment muscles and soft tissue in the lower extremities.
Fig. 1.
Preoperative computed tomography image. Coronal view of a computed tomography image showing a 3.5-cm anterior compartment muscle defect of the right lower limb (bone grafting was performed later through orthopedic surgery for the tibia defect).

Fig. 2.
Intraoperative clinical images. (A) Design of a vastus lateralis (VL) chimeric anterolateral thigh free flap (cALT-FF). (B) Harvested VL cALT-FF. (C) Clinical photograph revealing a 6-cm-long composite soft tissue defect with plate exposure, after the debridement. (D) An immediate postoperative photograph after the flap was inset.
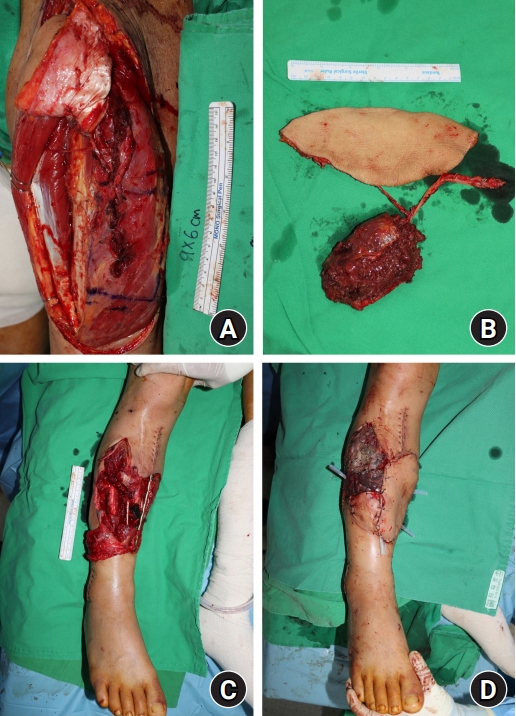
Fig. 3.
Scheme of the surgery. (a) This preoperative image represents a 6-cm muscle and soft tissue defect with plate exposure after the debridement. (b) On the other side (left) of the thighs, the chimeric anterolateral thigh free flap (cALT-FF) that had a vastus lateralis (VL) muscle component was harvested. (c) The fasciocutaneous component of the flap restored the soft tissue defect with plate exposure, and the VL muscle component was adjusted to suit the size of the muscle defect.

References
1. Manca M, Ferraresi G, Cosma M, Cavazzuti L, Morelli M, Benedetti MG. Gait patterns in hemiplegic patients with equinus foot deformity. Biomed Res Int. 2014;2014:939316.




2. Perry J, Burnfield JM. Gait analysis: normal and pathological function. 2nd ed. Thorofare, NJ: Slack Inc.; 2010.
3. Lin CH, Lin YT, Yeh JT, Chen CT. Free functioning muscle transfer for lower extremity posttraumatic composite structure and functional defect. Plast Reconstr Surg. 2007;119:2118-26.


4. Yazar S, Lin CH, Wei FC. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg. 2004;114:1457-66.


5. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453-8.


6. Yeap JS, Singh D, Birch R. A method for evaluating the results of tendon transfers for foot drop. Clin Orthop Relat Res. 2001;208-13.

7. Kim SW, Kim KN, Hong JP, Park SW, Park CR, Yoon CS. Use of the chimeric anterolateral thigh free flap in lower extremity reconstruction. Microsurgery. 2015;35:634-9.


8. Hallock GG. Simultaneous transposition of anterior thigh muscle and fascia flaps: an introduction to the chimera flap principle. Ann Plast Surg. 1991;27:126-31.