Standard incision and median nerve external neurolysis for recalcitrant carpal tunnel syndrome
Article information
Abstract
Purpose
Failed carpal tunnel surgery poses a challenge for the attending surgeon(s). Numerous revision techniques have been reported in the literature, with evidence of long-term improvement. However, studies exploring how early could symptomatic improvement be detected are scarce. The objective of this study was to identify the speed of symptom(s) recovery after a repeated decompression technique using an open standard incision and median external nerve neurolysis with no supplemental procedures.
Methods
Nine patients who underwent revision carpal tunnel surgery involving standard incision, external median neurolysis, and no supplemental techniques between June 2017 and June 2020, were included. Data regarding the preoperative Boston Carpal Tunnel Syndrome Questionnaire (BCTQ) score, Disabilities of the Arm, Shoulder and Hand score, visual analogue score, and grip strength were collected and compared with evaluation results at 3 months postoperatively.
Results
In all patients, severe adhesion of the median nerve with the surrounding soft tissue was confirmed intraoperatively. Compared with preoperative findings, 3-month evaluation of patients demonstrated a statistically significant improvement in the BCTQ symptoms score and pain score. All nine patients were satisfied with the procedure.
Conclusion
Standard incision and median nerve external neurolysis can be a good option for recalcitrant carpal tunnel syndrome patient who has an adhesion of the median nerve with surrounding soft tissue.
Introduction
Carpal tunnel syndrome (CTS) is the most common compressive neuropathy [1]. Surgical release of the transverse carpal ligament is successful in alleviating symptoms in 75% of patients, with minimal complications [2-5]. However, a subset of patients (3%‒20%) requires secondary surgery [6]. Indications for secondary surgery are related, in large part, to the persistence of preoperative symptoms and/or their recurrence [6,7]. While patient symptoms improve over the long term, management of failed carpal tunnel release (CTR) is challenging due to two major factors. First, despite the absence of comparative studies investigating the outcomes of primary and revision CTR, success rates following revision are assumed to be inferior [1,6,8,9]. Second, there is a lack of consensus regarding the optimal surgical management, evidenced by the various surgical techniques reported in the literature, ranging from simple release to those using complicated flaps and interposing tissue [6,8,10,11]. These perioperative challenges affecting patient consultation are also encountered when opting for the simplest technique—namely, repeated decompression without added procedures—due to the limited number of studies exclusively addressing its outcomes [6,12].
Despite the positive outcomes in the long-term improvement of patients, there have been few studies reporting the speed of postoperative recovery of symptoms and functional recovery following a revision surgery, which both constitute an important aspect of patient satisfaction and preoperative consultation owing to loss of function reflected in the presenting symptoms [1,6,8-11]. Therefore, the present study aimed to determine the speed of symptom(s) improvement and early functional recovery pattern(s) following a simple revision technique that included repeated decompression through a standard incision and median nerve external neurolysis without any additional procedures. Accordingly, we performed a case series study involving patients who underwent a revision CTR surgery using this technique and compared their baseline preoperative findings with 3-month postoperative outcomes according to various clinical and scoring systems.
Methods
Ethics statement: This study was approved by the Institutional Review Board of Asan Medical Center in Seoul, Korea (No. 3010-3523). The study was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
1. Study design and patient characteristics
From the authors’ database of CTS patients, 16 patients who presented to the outpatient clinic with recurrence or persistence of symptoms after undergoing primary CTR were identified. Adult patients aged >18 years who underwent repeated decompressive surgery through a standard incision with external median nerve neurolysis without supplemental procedures and had a complete electronic chart (specifically, 3-month postoperative follow-up) were included. Individuals with incomplete data (n=4), presence of degenerative cervical spine disease, history of rheumatoid arthritis, history of trauma to the wrist, or revision surgery using a different technique (n=2) were excluded. Of the remaining 10 patients, one was excluded due to an intraoperative finding, which was a median nerve neuroma requiring excision and nerve grafting. Therefore, the case series included nine patients who underwent surgery using this technique between June 2017 and June 2020. Electronic charts were reviewed and the following information was collected: age, sex, hand dominance, classification of patients (recurrent or persistent), intraoperative findings during revision surgery, and clinical assessment notes.
2. Operative procedure
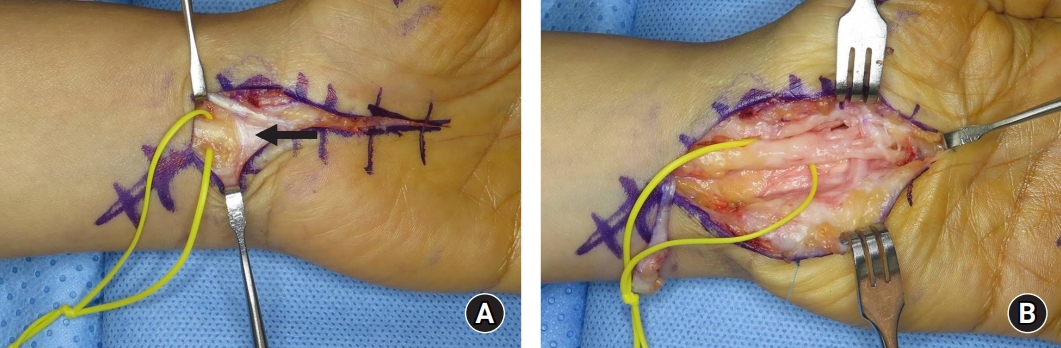
Surgical procedures were performed as day-surgery cases under loupe magnification and local anesthesia. The surgical technique was identical in all included patients. The choice of incision was a standard incision as described by Taleisnik (Fig. 1A) [13,14]. After skin incision, the transverse carpal ligament and palmar aponeurosis were completely released to gain full exposure of the carpal tunnel contents, where potential causes of recurrence and persistence could be identified and addressed. During the procedure, the median nerve and its palmar cutaneous branch were identified and examined for laceration, evidence of ongoing compression, or presence of neuromas. This was followed by external neurolysis of the median nerve; external neurolysis involved liberating of the median nerve by extensive dissection from the scar tissue or adhesion (Fig. 1B). In this procedure, the epineurium is not dissected. The procedure was completed by skin closure and application of compressive dressing.
3. Assessment
At both the preoperative and 3-month postoperative evaluations, the grip strength and Patient Reported Outcome Measures (PROMs) were collected from clinical assessment notes. Assessment of grip strength was measured using a dynamometer and reported in kilograms. The PROMs utilized included the Boston Carpal Tunnel Questionnaire (BCTQ), the visual analogue score (VAS) and the Disabilities of the Arm, Shoulder, and Hand (DASH) score. The BCTQ is a self-administered form developed specifically for CTS. The BCTQ included two subsections for symptoms (BCTQ-SS) and function (BCTQ-FS). The DASH score consists of 30 items that evaluate abilities to perform specified activities (21 items) or symptoms (9 items) [15,16]. Patient satisfaction was also scored on a 5-point scale, in which a score of 1 indicated being very unsatisfied and a score of 5 indicated being very satisfied. In the authors’ practice, a follow-up nerve conduction study is usually not requested unless new symptoms emerge in patients during follow-up, indicating persistence or a new complaint.
4. Statistical analysis
Data are expressed as medians and interquartile ranges (IQRs). The Wilcoxon test for paired samples was used to compare preoperative and postoperative PROMs and grip strength in the patients. Differences with p-values of <0.05 were considered to be statistically significant.
Results
1. Patient characteristics and operative findings
For this study, nine consecutive patients (10 hands) who underwent revision CTR at the authors’ center were recruited, among whom three were male and six female, with an average age of 60 years (range, 45‒85 years). The affected side was left in six hands and right in four.
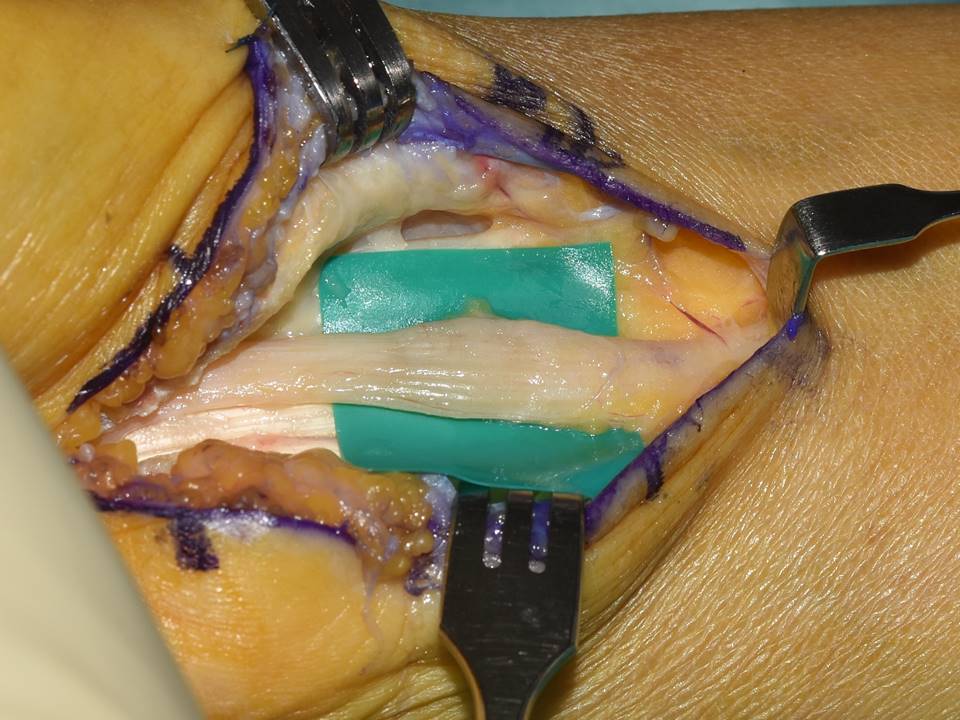
The patients’ demographic characteristics and operative findings were described in Table 1. For all patients, intraoperative findings included diffuse adhesions and synovitis around the median nerve. Four of five patients with persistent type had a reformed transverse carpal ligament. We identified hourglass constriction (hourglass sign) in one patient with recurrent type (Fig. 2).
2. Postoperative outcomes
A statistically significant improvement was observed in the median values of two outcome measures; the BCTQ-SS and VAS. The median preoperative BCTQ-SS score changed from 2.6 (IQR, 1.9‒2.9) to 1.8 (IQR, 1.4‒2.0) at the 3-month evaluation (p=0.01). The median preoperative VAS changed from 5 (IQR, 4‒6) to 2.5 (IQR, 2‒4) (p=0.007). Although other outcome measures demonstrated improvement, the differences were not statistically significant. The median BCTQ-FS improved from 2.4 (IQR, 1.8‒3.9) to 1.8 (IQR, 1.8‒2.3) (p=0.8). The DASH score improved postoperatively, as the median changed from 46 (IQR, 20‒64) to 31 (IQR, 27‒41); however, this change was not statistically significant (p=0.16). Median grip strength changed from 13 kg to 18 kg; however, this also was not a significant change (p=0.9). Nevertheless, all nine patients were satisfied with the procedure (Table 2).
DISCUSSION
In the present case series, we found that for revision CTR, repeated decompression using a standard incision with median nerve external neurolysis was a satisfactory procedure and was associated with early improvement in patient symptoms. This was evident in the 3-month postoperative evaluation, which exhibited a statistically significant improvement in symptom-related PROMs (the BCTQ-SS and VAS). This procedure was also associated with considerable satisfaction among patients, despite incomplete functional recovery.
In general, management of patients with failed CTR is much more challenging than that of patients with primary CTS [6]. If surgery is planned, careful council should be performed to emphasize the possibility of incomplete relief of symptoms and even worsening neurologic symptoms. Furthermore, the optimal surgical method should be selected after careful consideration of each patient’s condition. Although our study revealed satisfactory outcomes using a standard incision with median nerve external neurolysis, this procedure should be used only after other techniques have been ruled out as options. When neuroma is suspected due to definite iatrogenic nerve injury, internal neurolysis under microscope in addition to external neurolysis is almost always required. After meticulous internal neurolysis of the injured fascicle, the transected nerve is transposed to the muscle interface or reconstructed with a short nerve graft [17].
As an alternative surgical option, tissue interposition flaps may be considered for patient who has previously undergone multiple surgical attempts or is suspected of having profound soft tissue problem. Despite the increased complexity of procedure and donor-site morbidity, those procedures provide a barrier between the median nerve and overlying soft tissue, effectively preventing adhesion and scarring of the median nerve [1,8,18-20]. Supplemental procedures, such as pedicled hypothenar fat flaps based on ulnar artery perforators, were used in 45 patients during a median follow-up of 45 months, with excellent/good outcomes reported in 94% of these patients despite resultant hyperesthesia at the incision site in all patients [18]. Alternatively, flexor tendon tenosynovial vascularized flaps were described recently as another option to prevent adhesion and scarring and were reported to have long-term outcomes of resolved pain in 98% and an improvement in tingling in 80%. As a complication, they were associated with flexor tendon adhesions and scarring [19]. Distant autologous means of covers were also described, with saphenous vein wraps being the most common. Although these wraps carried the risk for donor-site discomfort, they were reported to lead to pain relief in 100% of patients [20].
Subsequently, our revision technique, aiming to avoid donor-site morbidities, was devoid of additional procedures and relied on a standard incision providing appropriate exposure for assessment and management of the most common reported etiologies of persistent and recurrent CTS—namely, incomplete release of the transverse carpal ligament and scar formation [6,7,21,22]. Operative findings from our study strongly supported those etiologies of recalcitrant CTS. In our study, the most common intraoperative findings of patients with persistent type remained transverse carpal tunnel ligament. In patients with recurrent type, a compression of the median nerve due to adhesion and scar formation was observed intraoperatively. Long-term improvement of symptoms following a standard incision with median nerve external neurolysis has been reported in other studies. In a homogenous case series involving 13 patients with recurrent symptoms who underwent surgery using a similar technique, Duclos and Sokolow [23] reported a symptom(s) disappearance rate of 92% over an average of 27.5-month follow-up. More recently, over an average of 20-month follow-up of 14 patients with recurrent CTS treated with a similar technique, other authors reported a statistically significant improvement in QuickDASH scores, improvement in mean EuroQol 5-Dimension 3-Level (EQ-5D-5L) general health questionnaire scores, satisfaction among 13 patients, a net promoter score of 85, and lack of complications [11]. Neither of these studies, however, assessed the speed of symptom(s) recovery, which was the focus of the present investigation.
Our evaluation of patients 3 months postoperatively demonstrated a significant improvement in symptoms and pain. However, this was associated with no change in the BCTQ-FS, DASH score, or grip strength. Because we performed complete sectioning of the transverse carpal ligament, the mechanics of gripping and pinching were expected to be affected, thus limiting significant early improvement of function in our patients. Therefore, this incomplete recovery is not different from immediate and early postoperative function recovery following primary CTR [24,25]. In a prospective study by Katz et al. [24] involving 35 patients with a mean follow-up of 27 months following primary CTR, the assessment of function included grip strength and the BCTQ-FS. For these patients, the functional recovery at 3 months was characterized by a gradual improvement in the mean BCTQ-FS (2.79–2.10) and a decline in the mean grip strength, from a baseline of 21.8 to 11.8 kg. Additionally, a randomized controlled trial comparing the outcomes of open and endoscopic CTR reported that, at 3 months following open CTR, the grip strength had declined in a statistically nonsignificant manner from a preoperative mean of 31.2 to 29.9 kg [25].
Our study was limited by its retrospective design and small number of patients. However, because the rates of revision CTR are low in both the literature and at our center, the number of included patients was inherently small and the study design had to be retrospective. Another limitation was that long-term outcomes were not reported because we focused on addressing the speed of recovery and symptomatic improvement.
Conclusion
In patients with severe adhesion of the median nerve with surrounding soft tissue, a simpler approach for repeated decompression that includes a standard incision and external median nerve neurolysis with no added procedures was associated with a significant and rapid improvement in symptoms detectable at 3 months, and with considerable satisfaction. However, surgical candidates should be determined carefully after meticulous preoperative evaluation.
Notes
The authors have nothing to disclose.
Funding
None.