Evaluation of Hospital Avoidance at Department of Hand Surgery in Tertiary Hospital after Infectious Disease Outbreaks
Article information
Abstract
Purpose
This study was performed to compare the impact of hospital avoidance on the department of hand surgery at a tertiary hospital in Daejeon in the wake of the Middle East respiratory syndrome (MERS-CoV) and coronavirus disease 2019 (COVID-19) outbreaks.
Methods
This is a retrospective comparative study of patients who were treated at the department of hand surgery in a tertiary hospital of a local community. We analyzed patients who were treated during the MERS-CoV and COVID-19 outbreaks. Controls included patients who were treated in the previous year during the same months. The number of outpatient visits and surgeries were compared to examine the difference from the previous year during the epidemic period of each infectious disease, and changes in demographic factors, the ratio of first and second visits, and the ratio of scheduled and emergent surgeries.
Results
Under MERS-CoV, outpatient visits decreased by 9.7% and surgeries by 26.5% for 3 months. In June 2015, when MERS-CoV was widespread in Daejeon, the number of outpatients and surgeries dropped by 25.3% and 42.8%, respectively. During COVID-19, outpatient visits decreased by 4.3% and surgeries increased by 2.9%. However, when COVID-19 was most prevalent in Daejeon, the number of outpatients and surgeries increased by 36.6% and 31.1%, respectively.
Conclusion
The impact of the COVID-19 outbreak in 2020 on the department of hand surgery at a tertiary hospital in Daejeon was limited, compared to the MERS-CoV epidemic in 2015, which can be attributed to improved infectious disease response capabilities.
INTRODUCTION
Coronavirus or coronavirus disease-19 (COVID-19), which is an infectious respiratory disease, was first reported in Hubei, China, in December 2019, and has since spread worldwide [1]. As the number of infections increased significantly, the World Health Organization (WHO) declared COVID-19 a “pandemic” in March 2020 [2]. In Korea, the COVID-19 outbreak occurred sporadically following an inflow of international tourists after mid-January 2020, but from mid-February 2020, a large-scale epidemic outbreak was reported in Daegu and Gyeongsangbuk-do, with the infectious disease crisis alert raised to “serious” [3]. In Daejeon, there were cases reported by international tourists or sporadic community infections until May, with the total number of infections rising to 45, which was relatively well-controlled [4]. However, the number of infections increased rapidly in June, to 75 cases [4]. Subsequently, the number of infections decreased to 45 cases in July, and after one case of infection on June 18, 2020, it entered a lull until the second wave of the epidemic in mid-August [4].
Meanwhile, 5 years ago in May 2015, the Middle East respiratory syndrome (MERS-CoV) was first reported in Korea and the entire nation was in the grip of fear [5]. It lasted for approximately 8 months from May to December 2015, and a total of 186 infected cases were confirmed, resulting in 38 deaths, with a fatality rate of 20.4% [5,6]. Owing to the poor initial response and weak domestic medical delivery systems, large-scale secondary and tertiary infections were reported around hospitals, causing great social chaos [6,7]. In the metropolitan city of Daejeon, the infection spread mainly through hospitals [8,9]. Since the first confirmed case in Korea on May 20, 2015, the epidemic began spreading in June, with a total of 182 confirmed cases by June 30, 2015 [8,9]. Among them, 82 (45.1%) were hospitalized patients, 64 (35.2%) were related to hospital visits, and 36 (19.8%) were hospital-related workers, such as medical staff [8,9]. As a consequence of hospital avoidance triggered by MERS-CoV, the number of inpatients and outpatients decreased by 22% and 23%, respectively, in June 2015 [10,11]. The decrease in revenue was estimated at about 207 billion Korean won (KRW) in tertiary hospital, 271 billion KRW in general hospital [10,11].
The authors are hand surgeons working at the department of hand surgery at a tertiary general hospital located in Daejeon and have experienced both MERS-CoV and COVID-19 infections. From the experience of MERS-CoV, not only the national quarantine system but also the quarantine capabilities at hospitals have been greatly developed. In addition, public awareness of infectious diseases rose significantly compared to the past [12]. In 2015, in the wake of the MERS-CoV epidemic, scheduled surgeries were canceled and the number of outpatients decreased by an average of more than 10% in the hospital where the authors worked. Meanwhile, although COVID-19 began to spread in the Daejeon area from May 2020, raising a sense of crisis among citizens, it did not lead to a decrease in the number of patients, as it did 5 years ago. Therefore, in this study, we evaluated and compared the impact of each infectious disease on the department of hand surgery at a tertiary hospital in the local community.
MATERIALS AND METHODS
This study is a retrospective comparative study of patients who were treated at the department of hand surgery in a tertiary hospital in a local community. This study was approved by the Institutional Review Board of Chungnam National University Hospital (No. CNUH 2020-08-39). Informed consent was waived because of the retrospective nature of the study and the analysis used anonymous data. COVID-19 was first reported in May and peaked around June 2020 in the community where the hospital is located. The authors analyzed patients who were treated at the department of hand surgery from May to July 2020, with patients who underwent treatment in May to July 2019 considered as controls. Since MERS-CoV was first reported in the same community in May 2015 and peaked around June the same year, the authors analyzed patients from May to July 2015, with patients treated from May to July 2014 considered as controls. The inclusion criteria were as follows: (1) patients aged 18 years or older, (2) patients who underwent treatment at the department of hand surgery, and (3) patients with trauma or disease limited to the upper extremities. Patients who received treatment for the shoulder joint area or patients with malignant tumors were excluded.
As the primary outcome, we analyzed the changes in the volume of outpatients and surgeries at the department of hand surgery under each epidemic period and compared it to the controls. As secondary outcomes, we analyzed patients’ demographic factors, the ratio of first and second visits, and changes in scheduled and emergent/urgent surgeries. Scheduled surgeries are those that allow for adjustment of the surgical schedule, such as ulnar impaction syndrome, triangular fibrocartilage rupture, carpal tunnel syndrome, cubital tunnel syndrome, and benign tumor. Emergency and urgent surgeries were defined as cases that could affect prognosis if the schedule was delayed, such as a fracture, tendon rupture, nerve injury, or infection.
Statistical analyses were performed using the IBM SPSS Statistics ver. 20.0 (IBM Corp., Armonk, NY, USA). Descriptive analyses were conducted employing the mean and standard deviation. For categorical variables, the frequency and percentage of each category were presented, and a chi-square test was performed. For continuous variables, mean and standard deviation were provided, and an independent sample t-test was performed. A p-value of less than 0.05 was regarded as significant.
RESULTS
1. MERS-CoV epidemic and outpatient volumes at the department of hand surgery
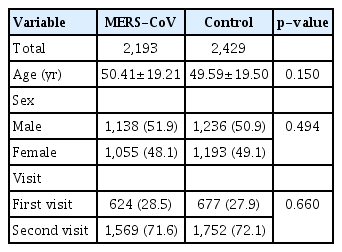
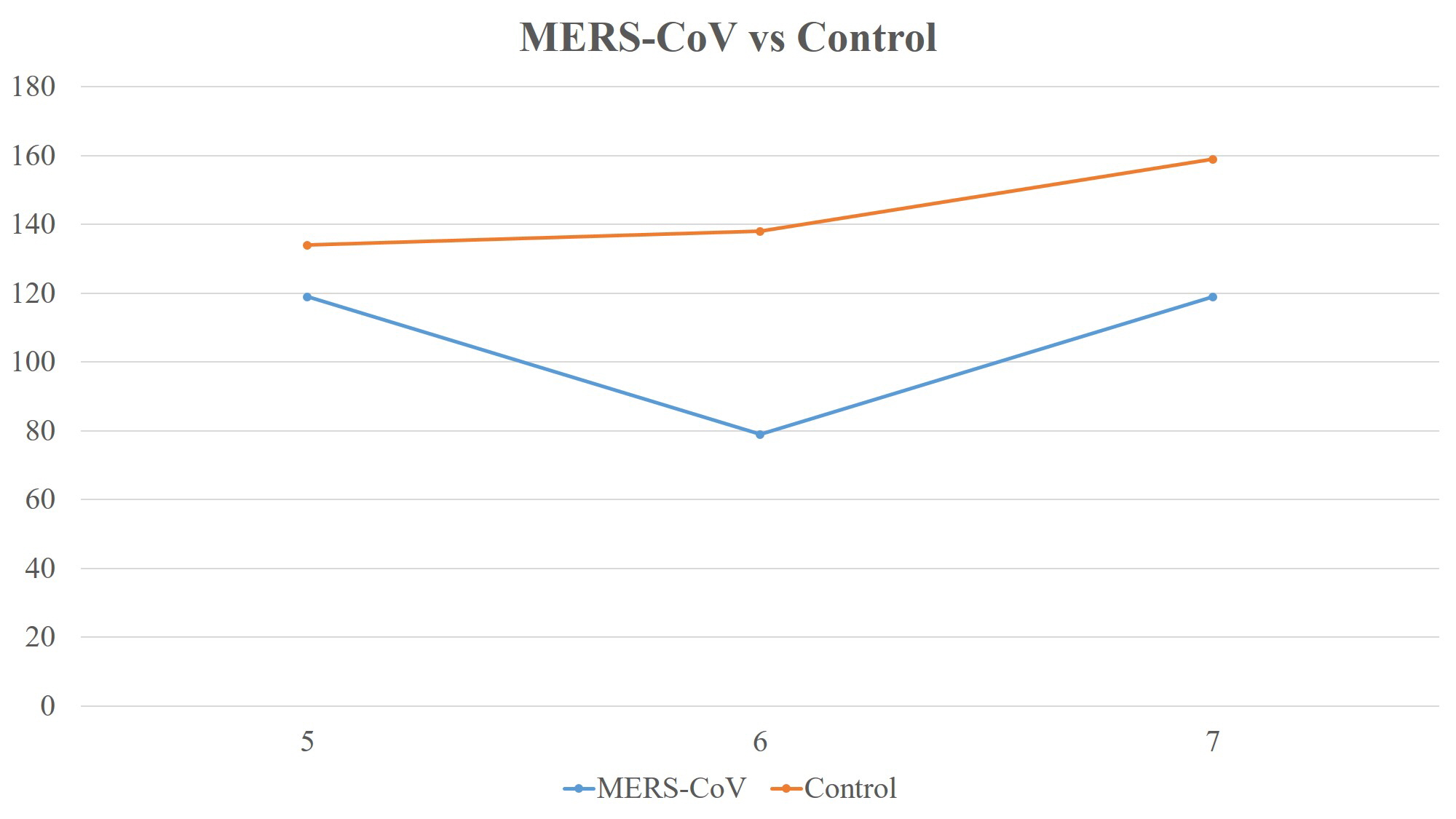
In May 2015, there was no change in the number of outpatients compared to the same month in the previous year. However, in June, when MERS-CoV began to spread, the number of outpatients decreased by 25.3% from the corresponding month of the previous year. In July 2015, it showed a recovery, with only a 3.9% decrease in outpatients compared to the same month in the previous year (Fig. 1). During the 3 months of the MERS-CoV epidemic, there was a 9.7% reduction in outpatient volumes compared to the previous year. There were no significant differences in age, sex, and the ratio of first and second visits (Table 1).

Middle East respiratory syndrome (MERS-CoV) epidemic and outpatients’ volume at the department of hand surgery.
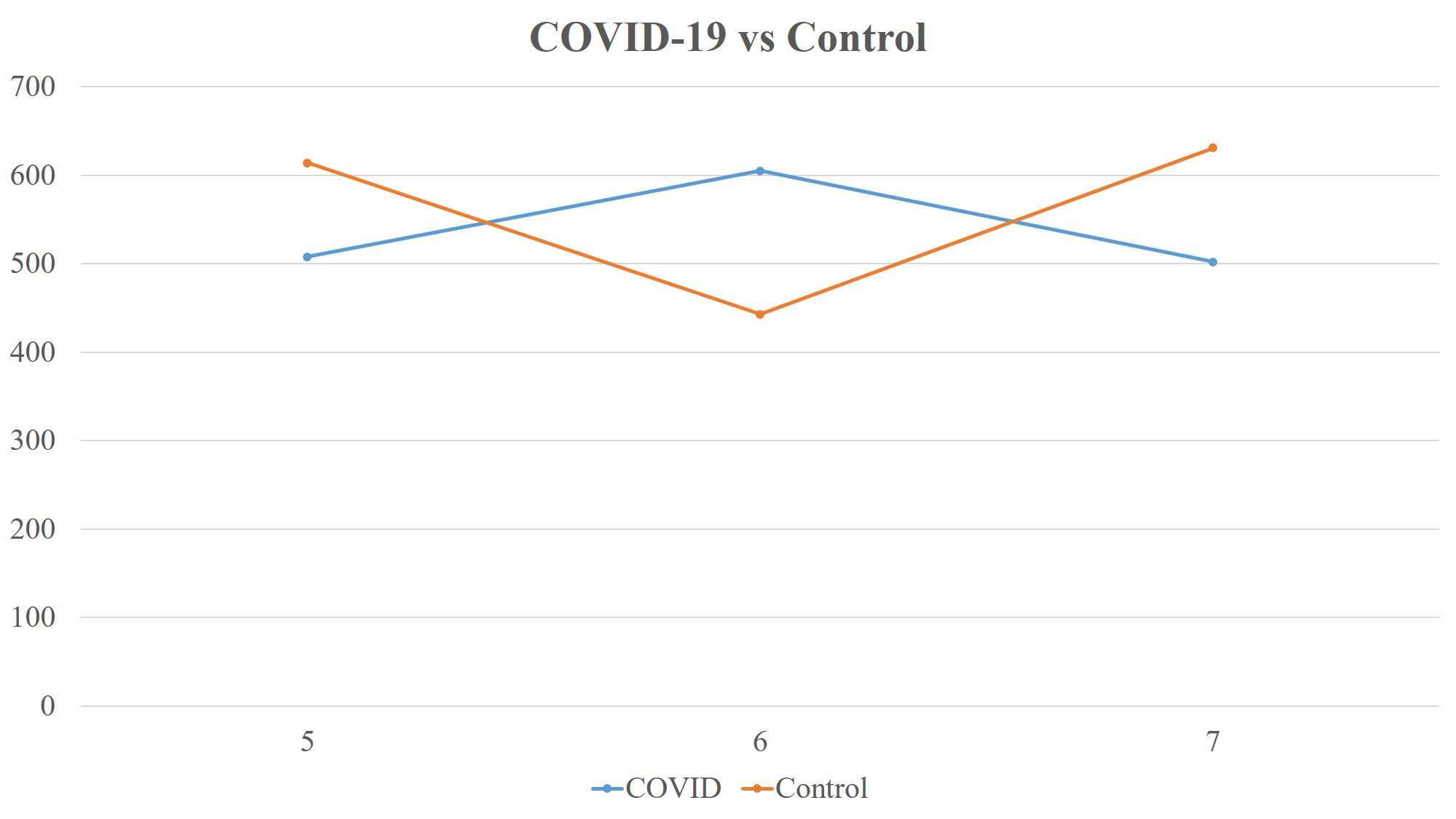
2. COVID-19 epidemic and outpatient volumes at the department of hand surgery
In May 2020, the number of outpatients decreased by 17% compared to the same month in the previous year. In June, when COVID was widespread in Daejeon, outpatient visits increased by 36.6%, when compared to the corresponding month of the previous year. In July 2020, it decreased by 18.1%, compared to the previous year (Fig. 2). During the 3 months of the COVID-19 epidemic, outpatient volumes contracted by 4.3% compared to the previous year. The average age of outpatients was younger during the COVID-19 epidemic than in the previous year (COVID-19, 51.06±16.57 and control, 52.63±17.16; p = 0.007). There were no significant differences in sex or the ratio of the first and second visits (Table 2).
Coronavirus disease 2019 (COVID-19) epidemic and outpatients’ volume at the department of hand surgery.
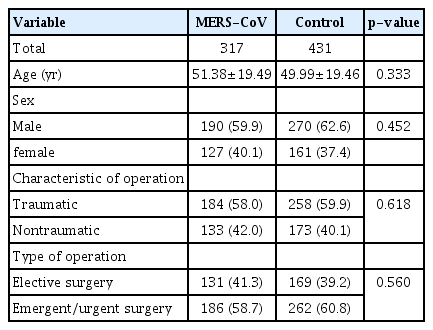
3. MERS-CoV epidemic and the volume of hand surgeries
In May 2015, the number of hand surgeries diminished by 11.2%, compared to the corresponding month of the previous year. In June 2015, when MERS-CoV was prevalent, hand surgeries dropped sharply by 42.8% and subsequently showed recovery with a decrease of 25.2% in July (Fig. 3). During the 3 months of the MERS-CoV epidemic, the number of hand surgeries plummeted by 26.5% compared to the previous year. There were no significant differences in age, sex, or the ratio of scheduled to emergency or urgent surgeries (Table 3).
4. COVID-19 epidemic and the volume of hand surgeries
In May 2020, there was a marginal change compared with the corresponding month of the previous year. However, in June 2020, when COVID-19 was prevalent in Daejeon, the number of hand surgeries increased by 31.1% compared to the same month of the previous year. In July, the number of hand surgeries decreased by 21.1% year-on-year, and emergent/urgent surgeries reduced significantly from 45.7% to 36.5%. During the 3 months of the COVID-19 epidemic, there was a marginal increase of 2.9 % in the volume of hand surgeries compared to the previous year, although there was a significant drop in emergent/urgent surgeries (Fig. 4). Additionally, the age of patients who underwent hand surgeries was significantly lower during the COVID-19 epidemic period, although there were no significant differences between sexes (Table 4).
DISCUSSION
In view of hospital avoidance triggered by the MERS-CoV epidemic, outpatient visits decreased by 9.7% and the number of surgeries dropped by 26.5% for 3 months at the department of hand surgery. In June 2015, when fear surrounding MERS-CoV reached its peak, the number of outpatients and surgeries decreased by 25.3% and 42.8%, respectively, showing a more striking change. There were no significant differences in demographic factors, first/revisit ratio, and emergency/urgent surgery ratio, compared to the previous year, which suggested that the decrease can be attributed to hospital avoidance following the infectious disease outbreak. However, the impact of COVID-19 has been limited. The decrease in the number of outpatient visits for 3 months was 4.3%, and surgeries showed a 3% decline. In June 2020, when COVID-19 was widespread in Daejeon, the number of outpatients increased by 36.6% and surgeries by 31.1%. In addition, the average age of outpatients was significantly lower than in the previous year, and the number of revisiting patients decreased and the number of first-visit patients increased. The ratio of emergency and urgent surgeries and the mean age of patients who underwent surgery were also significantly lower. These changes could have been driven by other factors, such as social distancing and limited activities, rather than by hospital avoidance.
MERS-CoV and COVID-19 are both caused by coronavirus, which is enveloped RNA viruses [13]. The difference is that MERS-CoV has a higher mortality rate, but is less infectious than COVID-19 [13]. However, due to its high infectivity, the number of deaths from COVID-19 has far exceeded the cumulative deaths from MERS-CoV. Given the highly infectious nature of COVID-19, it could be expected that hospital avoidance would be greater than that of MERS-CoV, but this was not the case.
The authors believed that hospital avoidance could have been minimized for the following reasons under the COVID-19 epidemic. First, the government and hospitals have actively promoted individual precautions, and the public had a high practice rate. According to a report comparing the implementation rate of social distancing and personal precautions for a total of 4,011 subjects during the MERS-CoV and COVID-19 epidemics, the ratio of wearing a mask and practicing hand hygiene was improved from 15.5% to 78.8% and from 60.3% to 80.2%, respectively, during the COVID-19 epidemic, which was a significant increase compared to that during the MERS-CoV epidemic [12]. The marked increase in mask wearing may have been a factor in reducing patients’ anxiety when visiting a hand surgeon. In addition, since all medical staff, patients, and their families are obliged to wear masks in the hospital, the anxiety of nosocomial infection could have been reduced. The second factor was the hospital’s efforts to minimize nosocomial infections. Of the total 182 MERS-CoV-confirmed patients up to June 30, 2015, 82 (45.1%) were hospitalized or visited the hospital, and 64 (35.2%) visited the hospital as a patient’s family or other non-family members, and 36 (19.8%) were hospital-related workers such as medical staff [8]. Since most were hospital-related infections, it is possible that hospital avoidance was more prominent. Based on the lessons from MERS-CoV, the hospital has implemented measures to prevent nosocomial infections in response to the outbreak of COVID-19. Visiting hospitalized patients was completely prohibited, and entry into the ward was allowed only for one guardian with a pass. In addition, the hospital operated a drive-and-walk-through testing station to conduct full-scale COVID-19 investigations on all prospective patients who required hospitalization. At the ninth meeting of the Emergency Committee convened by the Director-General under the International Health Regulations, the WHO attributed the spread of MERS-CoV in Korea to two factors [14]. One was the lack of hospital-acquired infection prevention and control measures, and the other was the culture of many visitors and patients’ families staying in the hospital room [14], which has since been overcome. These improvements play a role in not only reducing actual nosocomial infections but also relieving the anxiety of patients visiting outpatient clinics and hospitalized for surgery. The third factor was transparent information disclosure. At the beginning of the MERS-CoV outbreak, patients’ movement routes and the name of the medical institution that they visited were not disclosed. As it was not decided whether to disclose MERS-CoV-related information until early June 2015, unverified information spread through the Internet and social network services, spreading vague anxiety and fear among the people [7]. This prevented patients from visiting the hospital. Subsequently, the Korea Centers for Disease Control and Prevention specified “resolving public anxiety through prompt, accurate, and transparent information disclosure” in the basic crisis management policy. They transparently disclosed the patients’ movement route and the medical institute through which the patients passed. Although there were privacy concerns, the authors believe that these measures are effective in reducing patients’ avoidance of hospitals and helps maintain the function of the department of hand surgery under the COVID-19 situation.
The limitations of this study are as follows: First, since it was a retrospective study during the period when each infectious disease was declared an epidemic, it did not reveal the exact cause of patients’ hospital avoidance. Therefore, a survey or prospective study is required. Second, in the case of MERS-CoV, it started to spread in Daejeon within a month after it was first reported in Korea, but in the case of COVID-19, it spread in Daejeon 5 months after its outbreak in Korea, which could have helped minimize hospital avoidance. Third, this study was a single-center study conducted at the department of hand surgery in a tertiary hospital, and a multicenter study will be needed to generalize the results of this study.
CONCLUSION
The impact of the COVID-19 outbreak in 2020 on the department of hand surgery at a tertiary hospital located in Daejeon was limited compared to the impact of the MERS-CoV epidemic in 2015. This can be attributed to improved infectious disease response capabilities, such as the government and hospital’s active promotion of personal precautions, the high public practice rate, hospitals’ efforts to minimize nosocomial infections, and transparent information disclosure. If the treatment time is delayed in hand surgery, the prognosis of the patients may be adversely affected, and there may be various problems such as additional medical expenses in the future. Therefore, it is important to minimize hospital avoidance by improving quarantine conditions and creating an environment where patients can visit a hand surgeon in a timely manner, in the event of the outbreak of another infectious disease in the future.
Notes
The authors have nothing to disclose.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Science and ICT) (Grant No. 2019R1C1C100396712).