광범위 두 번째 등쪽 손허리 동맥 천공지 피판을 이용한 제1수지 간부의 재건
Reconstruction of the First Web Space Using the Wide-Second Dorsal Metacarpal Artery Perforator Flap
Article information
Trans Abstract
Purpose
This study evaluated the functional and aesthetic outcomes of a wide-second dorsal metacarpal artery perforator flap for reconstruction of the first web space of the hand. This flap sets the proximal edge of the extensor retinaculum as the distal limit.
Methods
We measured the preoperative and postoperative angles of the first web space and assessed the quality of the donor site scar in eight patients.
Results
The average flap size was 5.5 × 2.8 cm (range, 5.0 × 1.5 cm to 5.0 × 6.0 cm), and all flaps survived completely. The mean postoperative angle was 53°. The mean Vancouver Scar Scale score of the donor site was 4 points, and the patients had near-normal thickness and vascularity values. There was no distortion of the scar, and patients were satisfied with the scar appearance of the donor site.
Conclusion
The wide-second dorsal metacarpal artery perforator flap is a useful technique to reconstruct large defects of the first web space. It is easy to raise, thin, and pliable, and has excellent color and tissue matching.
INTRODUCTION
The thumb is critical to hand function, and complete loss (amputation) of the thumb represents a 40% loss of hand function according to impairment rating conventions [1]. Adequate first web space is significant for the function of thumb. A contracted web space restricts thumb function, and a proper web space is indispensable for thumb abduction, web space expansion, and thumb mobility [2]. Many etiologies can induce web contracture, including trauma, burns, infection, paralysis, ischemia, spastic conditions, and improper splinting [3]. Many surgical techniques have been established to release web contracture using skin grafting, local flaps (Z-plasty, four-flap, or five-flap technique), first dorsal metacarpal flap, fill-up web flap, lateral arm flap, cross arm flap, groin flap, reverse posterior interosseous artery flap, and skeletal traction [4-6]. Each of these methods has its own advantages and disadvantages, and a surgeon must consider the recipient site condition, technical difficulty, and donor tissue similarity to determine the best plan. Cases with large defects after releasing all contracted structures require flap coverage to restore good function. The optimal donor site for web space reconstruction should be thin and pliable, easy to harvest and match the recipient site.
In our institute, we reconstructed the first web space using the wide-second dorsal metacarpal artery perforator flap (w-SDMAP flap) technique. The purpose of this study was to evaluate the results of the w-SDMAP procedure and to confirm the usefulness of the flap.
MATERIALS AND METHODS
1. Patients
The w-SDMAP technique was performed for reconstruction of the first web space in eight patients, including seven males and one female, from May 2013 through March 2020. The mean age of the patients was 47 years (range, 25–69 years) and the average follow-up period was 18 months (range, 3–33 months). Five patients underwent elective flap surgery due to contracture of the first web space, and three patients underwent emergency flap surgery to reconstruct defects. All procedures were performed by a single senior surgeon. The angle of the web space was measured with a goniometer [2], and the quality of the donor site scar was estimated with the Vancouver Scar Scale (VSS), which consists of four variables: pigmentation, vascularity, pliability, and height [7,8] (Table 1).
The study was approved by the Public Institutional Review Board designated by Ministry of Health and Welfare (No. P01-202012-21-001). All patients provided informed consent for surgery and for the publication of data and images.
2. Surgical techniques
All procedures were performed under brachial plexus block and pneumatic tourniquet control. The patient’s extremity was draped with betadine solution. The first step was the preparation of the web for flap transfer. In patients with web defects, sufficient debridement and marginal trimming were performed. In the case of web contracture, a linear skin incision was made perpendicularly through the dorsum of the first web to the palm. In most cases, the deep structures were contracted, and it was necessary to release the adductor pollicis muscle and first dorsal interosseous muscle. After sufficient myotomy, the web space was maintained by two parallel Kirchner wires inserted from the first metacarpal bone into the second metacarpal bone.
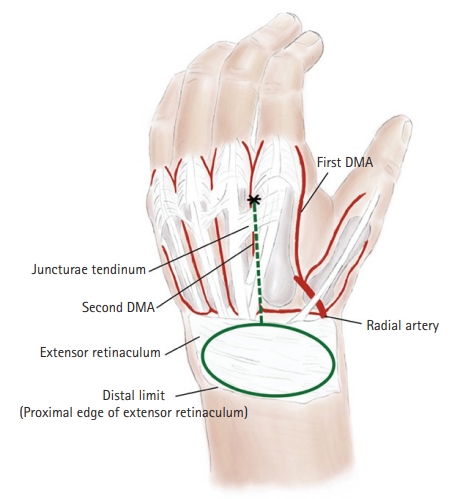
Subsequently, the size of the defect was measured, and the flap was designed. The selected perforator was marked at the metacarpal neck area, representing the pivot point. The proximal edge of the extensor retinaculum was set as the distal limit of the flap (Fig. 1). The long axis of the flap was mostly designed in a transverse fashion. After a tourniquet was inflated to 250 mmHg, the designed flap was incised with a No. 15 blade. The flap was then elevated from the plane of the extensor retinaculum and dissected distally to the pivot point at the metacarpal neck around the juncturae tendinum. It was not necessary to use color doppler ultrasonography to identify or visualize perforator vessels because of their consistent location, and the pedicle contained adequate adipofascial tissues for sufficient venous drainage. Elevation of the flap was continued to the proximal edge of the extensor retinaculum, and flap harvesting was completed. The flap was transferred to the recipient site through a subcutaneous tunnel, ensuring that the pedicle was not kinked or disrupted. After repositioning the flap to its native position, the tourniquet was deflated, bleeding was controlled, and flap perfusion was confirmed. The flap was then transferred to the defective first web using the half-buried horizontal mattress suture method. The donor wound was closed directly or with a skin graft. A thumb spica splint was applied to preserve the first web space, and Kirchner wires were maintained for three to four weeks. After surgery, alprostadil (Alostin injection; Dongkook Medica, Seoul, Korea) intravenous infusion and hyperbaric oxygen therapy were administered for 7 days to prevent congestion and to ensure flap survival.
RESULTS
The mean flap size was 5.5 × 2.8 cm, with the smallest flap measuring 5.0 × 1.5 cm, and the largest flap measuring 5.0 × 6.0 cm (Table 2). All flaps were based on the w-SDMAP flap. Six flaps were designed in a transverse fashion, one flap was oblique, and one flap was rectangular. All flaps were transferred to the defective web space through a subcutaneous tunnel. The donor wounds of three flaps were closed directly, and five flaps required full-thickness skin graft (FTSG) or split thickness skin graft for closure. All flaps survived completely, and three of them survived following the salvage procedure. Two flaps required a subsequent defatting procedure. The mean postoperative angle of the first web space was 53º. The mean VSS score was 4 points (Table 2).
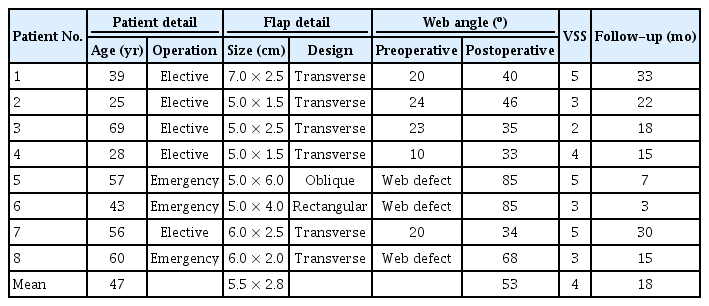
Patient and flap characteristics and postoperative assessment of the first web space and the donor site scar quality
1. Case 1
A 43-year-old man presented with a severe contact burn injury involving the first web space of the left hand. After a thorough escharectomy, the flexor pollicis longus was exposed partially (Fig. 2). To prevent contracture of the first web space, a w-SDMAP flap of size 5.0 × 4.0 cm was designed to cover the first web space defect. The flap was then elevated from the plane of the extensor retinaculum and extended to the proximal edge of the extensor retinaculum. Thereafter, the flap was transferred to the recipient site through a subcutaneous tunnel. The donor wound was closed with an FTSG from the upper inner arm. A thumb spica splint was applied to preserve the first web space. The flap survived completely, and the postoperative angle of the first web space was 85°. At the 3-month follow-up, the VSS score of the donor scar was 3 points. The patient had a slightly hyperpigmented scar with supple pliability. Additionally, there was no erythematous change or hypertrophic scarring on the hand dorsum scar. The scar was flat and the patient did not suffer from itching or pain.
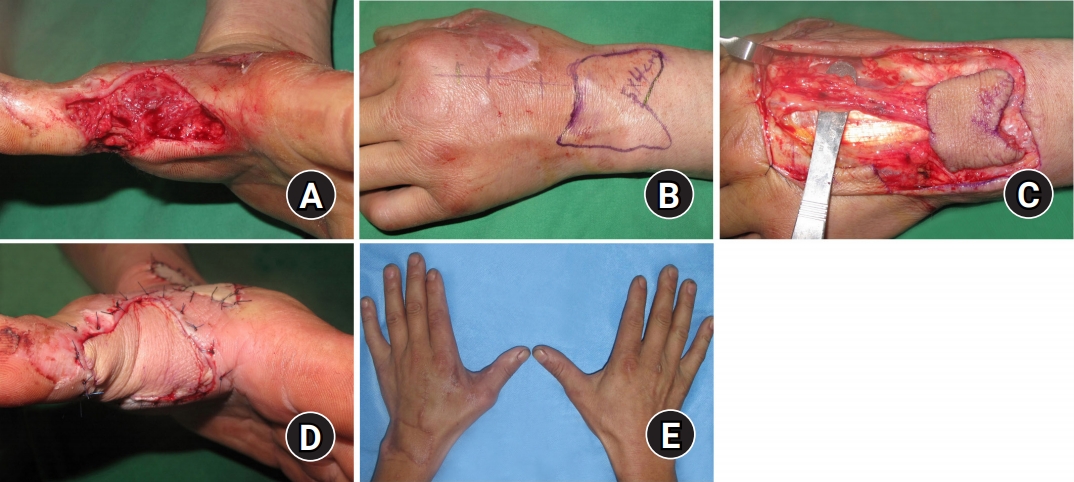
(A) Preoperative soft tissue defect of the first web space after a crush injury to the left hand. (B) A 5.0 × 4.0-cm rectangular wide-second dorsal metacarpal artery perforator flap with the proximal edge of the extensor retinaculum as the distal limit. (C) The flap is elevated and the pedicle is identified. (D) Immediate postoperative view. (E) Three months after surgery. The postoperative angle of the first web space was 85° and the Vancouver Scar Scale score was 3 points (pigmentation 2, vascularity 0, pliability 1, and height 0).
2. Case 2
A 25-year-old woman had a crushing injury with multiple fractures on her right hand (Fig. 3). Eleven months after the injury, the first web space had contracted. After sufficient myotomy, the web space was maintained using Kirchner wires. A 5 × 1.5-cm w-SDMAP flap was raised to cover the defect. The wound at the donor site was closed directly. The flap survived completely, and the postoperative angle of the first web space was 46°. At the 22-month follow-up, the patient was satisfied with the aesthetic results, and the VSS score was 3 points.

(A) Preoperative contracture of the first web space after a crush injury to the right hand. (B) A 5.0 × 1.5 cm wide-second dorsal metacarpal artery perforator flap with the proximal edge of the extensor retinaculum as the distal limit. (C) The flap is elevated and the pedicle is identified. (D) Immediate postoperative view. (E) Twenty-two months after surgery. The postoperative angle of the first web space was 46° and the Vancouver Scar Scale score was 3 points.
DISCUSSION
Adequate first web space is essential for hand function, and web space contracture can severely limit hand function. This study demonstrated that the w-SDMAP flap technique is useful in correcting large defects of the first web space. Aesthetic outcomes were acceptable, as measured by the VSS scores, and hand function was improved based on the postoperative improvements to the first web angle.
Many studies have assessed methods for measuring the angle of the first web space, but there is still no standardized method and no established normal angle. Fritsch used the intermetacarpal angle to measure the first web space and noted at least 45° as a normal web space angle [9]. Another study measured the distance from the thumbnail to the index metacarpophalangeal joint [10]. Jensen et al. [2] measured the first web space angle in normal volunteers using a goniometer and found that the mean angle was 100°. In this study, we outlined the web space on paper and then measured the angle using a goniometer [2]. Contracture of the first web space reduces the grasping ability of the hand and makes picking up small objects more difficult [2,11]. Many surgical approaches have been established to release web contractures, including skin grafts, local flaps (Z-plasty, four-flap, and five-flap technique), first dorsal metacarpal flap, fill-up web flap, lateral arm flap, cross arm flap, groin flap, reverse posterior interosseous artery flap, and skeletal traction [4-6]. Web space contracture can involve any combination of soft tissue components, including skin, fascia, intrinsic muscles, and ligaments. Accordingly, the principles of contracture release include adequate release of all tissues affecting contracture, lengthening of the contracted web, and resurfacing with additional tissue for a tension-free closure [11].
The dorsal metacarpal artery perforator (DMAP) flap was first described by Quaba and Davison [12], and it is a vascular island flap that is raised from the dorsum of the hand [13]. Because dissection is in the loose, areolar, and relatively avascular plane, which is superficial to the extensor paratenon, the DMAP flap is safe and easy to raise. Quaba and Davison [12] rotated the flap 90° in a propeller fashion when reconstructing the first web space. In this study, after releasing the first web space contracture, the coverage of the gross defect was needed. However, the traditional Quaba flap did not cover the palmar defect of the first web space. For this, a long pedicle was constructed using the adipofascial tissue between the perforator and flap, and then the defect was covered by moving the flap further away from the area where the perforator arose. Many anatomic studies have proven that the first and second dorsal metacarpal arteries are anatomically constant; thus, the flap has a safe pedicle source. The perforator arises just distal to the juncturae tendinum, and because it arises directly from the branches of the deep palmar arch, the DMAP flap can be raised even if there is no dorsal metacarpal artery [13-17]. Sebastin et al. [13] defined the indications of the DMAP flap in palmar defects up to the proximal half of the middle phalanx and dorsal defects up to the proximal distal interphalangeal joint. In that study, the distal edge of the extensor retinaculum was used as the distal limit for the DMAP flap because the distal DMAP can support the skin over the proximal half of the intermetacarpal space. A previous study set the distal edge of the extensor retinaculum as the distal limit. The average size of the flap was 4.6 × 2.3 cm, and the largest flap measured 6 × 4 cm [13]. In our study, the proximal edge of the extensor retinaculum was set as the distal limit, and all flaps survived perfectly. The average size of our flap was 5.5 × 2.8 cm, and the largest flap measured 5.0 × 6.0 cm. Our results demonstrate that a w-SDMAP flap can reconstruct the large first web space defect with a tension-free closure and a fingertip-width resurface defect. There are many methods to reconstruct the first web space, including free tissue transfer, such as a split groin flap, parascapular flap, lateral arm flap, and anterolateral thigh flap [18-20]. However, common drawbacks of these flaps are their bulkiness, mismatch of color and texture, microsurgical skill requirements, long recovery time, and postoperative immobilization [21]. By comparison, the harvest of the DMAP flap is fast and easy because it does not require microsurgery. An important goal of soft tissue reconstruction in hand defects is to regain normal or near-normal motion [22]. This requires thin, pliable tissue that allows thumb flexion and abduction. Another important consideration in selecting the tissue source is the principle of cosmetic units and subunits. The hand itself is better than other donor sites because it has better tissue match, texture, elasticity, thickness, and superior recovery of sensibility, and provides a single surgical anatomic field [21-23].
The disadvantages of the DMAP flap are a scar on the dorsal hand and the possible requirement of a skin graft to cover the donor site defect. The hand is a very visible and crucial part of human interactions and nonverbal communication [24-26]. Therefore, hand aesthetics are important to patients and may be a key factor when determining the donor site and estimating donor site morbidity. w-SDMAP flaps belong to distally based flaps with a special concern on venous drainage. To prevent venous congestion, sufficient adipofascial tissues around pedicles would be necessary. This flap has two venous systems; superficial venous system that drains from superficial tissues and deep venous system that drains from the retinacular microvenous connection [27]. In this study, venous congestion occurred in three cases, and flap survival was ensured after the salvage procedure.
There are many methods to assess scar quality, and the VSS is a tool that is widely used in many studies [7] (Table 1). In this study, the mean VSS score was 4 points. Our patients had near-normal thickness and vascularity values, which represent hypertrophic and pathologic scarring [28]. There was no distortion of the scar, and patients were satisfied with the scar appearance of the donor site. Nevertheless, preoperative informed consent is mandatory for postoperative scars on the hand dorsum. Furthermore, it would be better to use the skin laxity of the hand dorsum for aged patients than for young patients who are sensitive to scarring. As with conventional DMAP flaps [13], a preoperative check for deep lacerations, severe contusions, or metacarpal fractures around the vascular pedicle is essential.
CONCLUSION
The w-SDMAP is a useful technique for reconstruction of the first web space that is easy to raise, thin and pliable, and has excellent color and tissue matching. In addition, a w-SDMAP flap can reconstruct a large first web space defect with a tension-free closure and a minimal resurface defect.
Notes
The authors have nothing to disclose.