Various hand tumors: over 20 years of clinical experience in Korea
Article information
Abstract
Purpose
Although the hand only constitutes 2% of the body, it is a site where a wide variety of tumors occur, and the results of surgery substantially impact its function. Therefore, an accurate diagnosis and appropriate selection of individual treatment strategies are very important. This study reviewed the diagnostic characteristics and clinical features of surgically treated hand tumors at our facility.
Methods
We retrospectively reviewed 65 patients who underwent surgery for suspected hand tumors at our institution between 2003 and 2020. Data, including patient demographics, diagnosis, pathology, type of surgery, comorbidities, and tumor characteristics (e.g., location and tumor size), were collected from medical records.
Results
In total, 59 (90.7%) and six patients (9.3%) were diagnosed with benign and malignant tumors, respectively. Ganglion cysts were the most common tumors (n=11), followed by vascular anomalies (n=10), epidermoid cysts (n=7), and glomus tumors (n=4). There were four cases of bone tumors (6.2%), including one chondroma, one chondrosarcoma, and two giant cell tumors. In 53 cases with an imaging workup, the pathological diagnosis was concordant in 44 cases. Of the nine cases with inconsistent results, eight were tumors located in the finger; this association was significant (p=0.048).
Conclusion
In this study, ganglion cyst and squamous cell carcinoma were the most common benign and malignant tumors, respectively, and four cases of bone tumors were found. Radiologic misdiagnosis was more frequent in finger tumors than in other tumors. Thus, hand tumors, especially those suspected to be malignant, should be assessed using a multidisciplinary approach.
Introduction
A tumor of the hand is a disease that hand surgeons often encounter. As a very sophisticated and functional body part, the diagnosis and treatment of bone and soft tissue tumors of the hand are important. Most tumors originate from soft tissue, and most of them show benign findings [1,2]; however, benign tumors of the hand are less common than in other sites, and some are rare [3,4]. Therefore, a diagnosis based solely on clinical features is difficult, requiring extensive knowledge. Only a few clinical studies have comprehensively addressed the characteristics and diagnosis of tumors or tumor-like lesions in the hand [1,5,6]. The purpose of this study is to find out the types of hand tumors in Korean and to review the diagnostic modality usually used. Thus, we reviewed the pathological diagnosis, clinical features, and imaging modality of 65 cases of hand tumors that were operated at our facility.
Methods
Ethics statement: This study was done under the approval of the Institutional Review Board of Keimyung University School of Medicine (No. DSMC 2023-06-020). Written informed consent was obtained from the patient for the publication of this article including all clinical images.
We retrospectively reviewed 65 patients who underwent surgery for a suspected hand tumor at Keimyung University Dongsan Medical Center from 2003 to 2023. Patient data were collected from an electronic medical record system. Primary bone and soft tissue tumors and tumor-like lesions of the hand were included, while skin tumors, infectious diseases, and reactive lesions were excluded. Data, including patient demographics, diagnosis, pathology, type of surgery, comorbidities, and tumor characteristics, such as location and tumor size, were collected from medical records. The location was classified as “bone of the hand” for bone tumors and as “finger, palm, or dorsum of the hand” for soft tissue tumors. Tumor size was defined as the maximum diameter of tumors on postoperative measurement.
1. Statistical analysis
Data are presented as mean±standard error of the mean. Statistical differences were assessed using the chi-square test by GraphPad Prism. A p-value of <0.05 was considered statistically significant.
Results
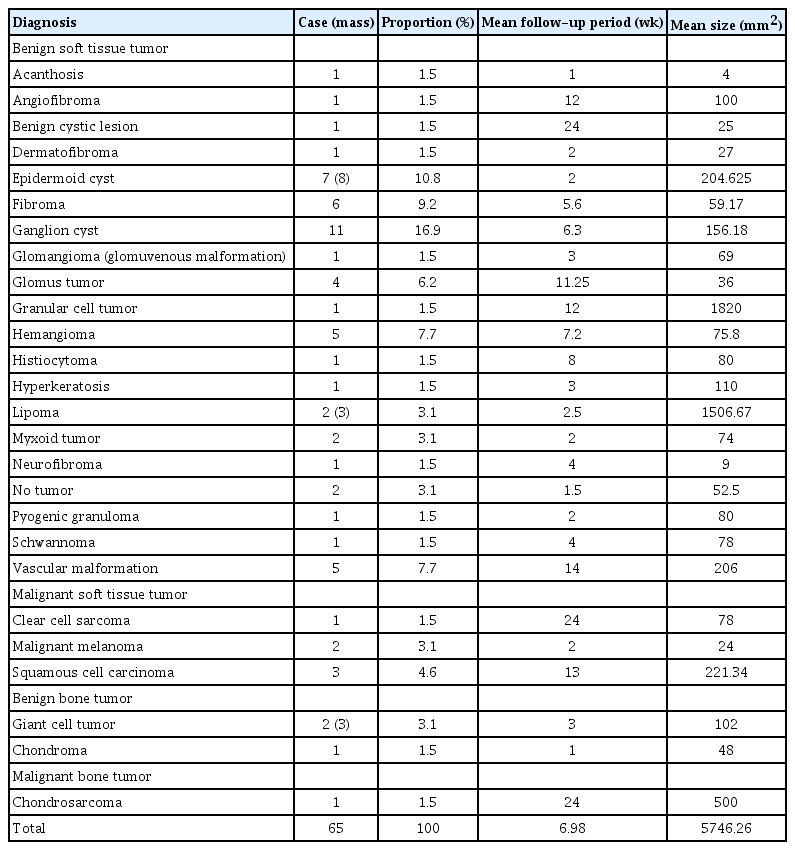
A total of 65 patients (28 male and 37 female) with a mean age of 48.9±19.8 years were analyzed. Of the hand tumors, 93.8% (n=61) were soft tissue tumors and 6.2% (n=4) were bone tumors. There were five malignant cases in soft tissue and one malignant case in bone tumor. The pathological diagnosis of the tumors of the patients included in the analysis is presented in Table 1. In soft tissue tumors, ganglion cysts were the most common tumor type in this study (16.9%, n=11). Vascular anomalies, including hemangiomas and vascular malformations, were observed (15.3%, n=10). Epidermoid cysts (10.7%, n=7) and glomus tumors (6.2%, n=4) were relatively common. In four cases of bone tumors, one chondroma, one chondrosarcoma, and two giant cell tumors were involved. Malignant cases included one chondrosarcoma, one clear cell sarcoma, two malignant melanomas, and three squamous cell carcinomas. In benign soft tissue tumors, granular cell tumors had the largest average size, followed by lipomas. Squamous cell carcinoma had the largest average size in malignant soft tissue tumors (Table 1).
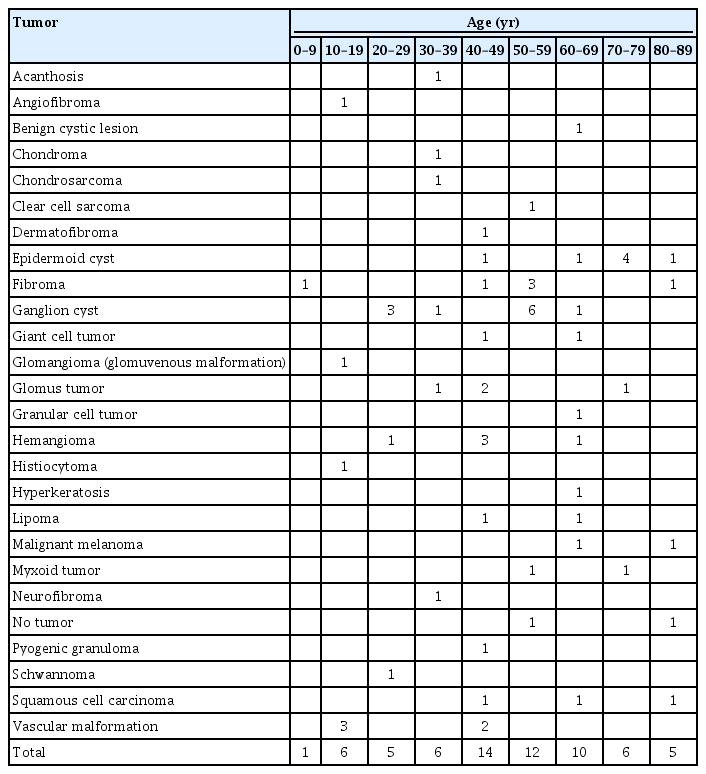
The number of pathological diagnoses per age group is shown in Table 2. Considering malignant lesions, the average age of the patients was 63.16±16.5 years; for benign lesions, the average age was 47.5±19.6 years. Patients presenting with malignant lesions had a higher mean age than those with benign lesions.
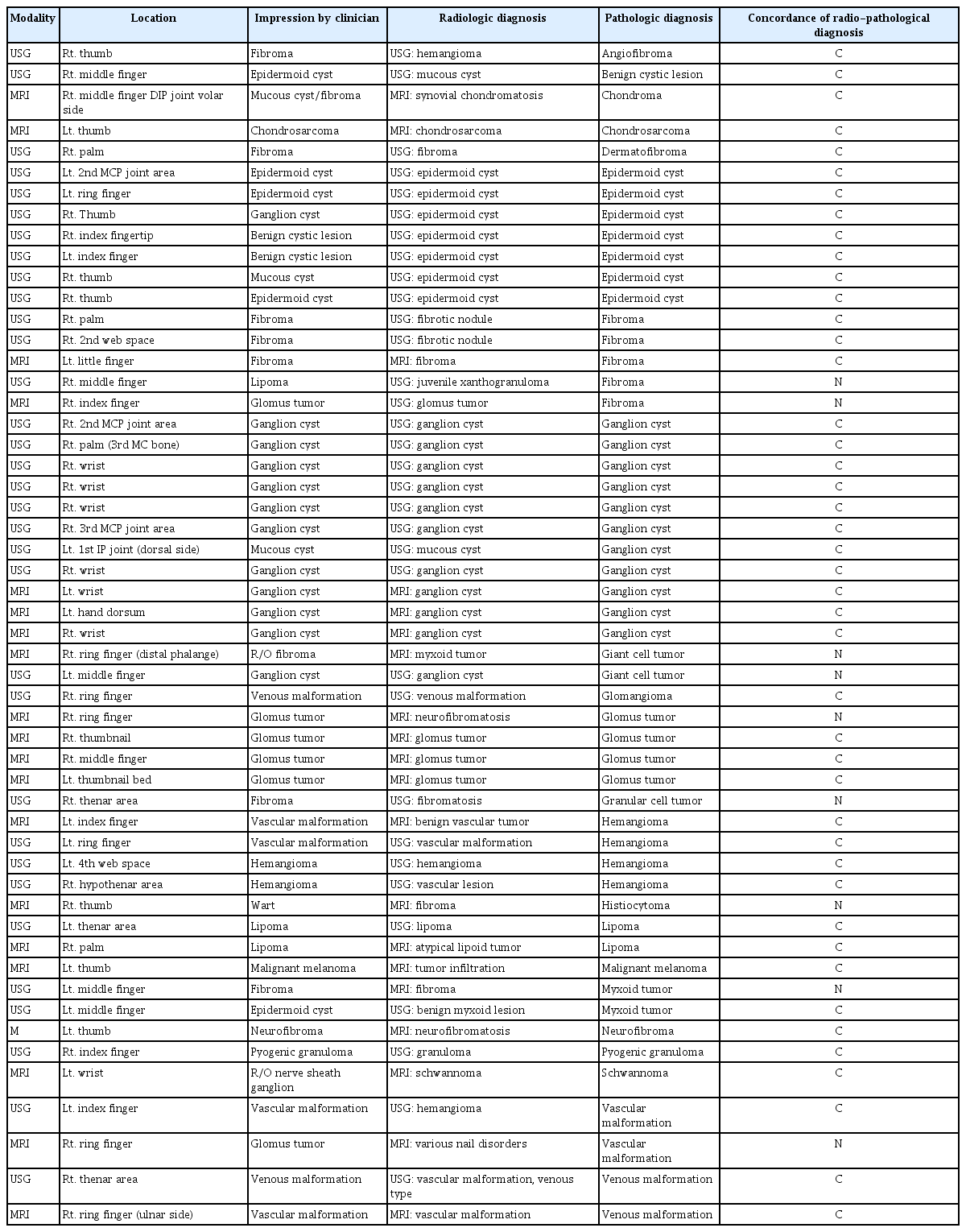
We performed a preoperative image workup when a soft tissue tumor located in the deep layer was suspected. Among the 53 cases in which imaging workup was performed, the pathological diagnosis was concordant in 44 cases (83.0%), and inconsistent results accounted for nine cases (16.9%) (Table 3). No significant difference in the accuracies of magnetic resonance imaging (MRI) and ultrasonography (USG) was observed; even in cases of finger tumors, no significant difference between the modalities was observed. Of the nine cases in which the results were inconsistent, eight were tumors located in the finger, and a significant difference was observed (88.9%, n=8 of 9; p=0.048, Pearson chi-square test).
Eight USG and three MRI scans were performed in 11 cases of ganglion cysts, which were all successfully predicted. USG was performed in seven cases of epidermoid cysts, all of which were successfully predicted. Vascular tumor cases, including hemangioma and glomangioma, were successfully predicted by USG and MRI in four and one case, respectively. USG and MRI were performed in two cases of vascular malformation, and MRI failed to predict in one case. Pain in the finger was reported in all four cases of glomus tumors; MRI was performed in all cases, and only one was misdiagnosed as neurofibroma. In two cases of giant cell tumors, MRI and USG were performed in each case, and neither could predict it accurately. In the case of fibroma, three USGs and two MRIs were performed in five cases, and two, which presented a mass in the finger, were diagnosed as glomus tumors and granulomas by MRI and USG, respectively.
Recurrence occurred regardless of the tumor type. Four cases of recurrence were found, including two cases of fibroma, one of myxoid tumors, and one of glomangioma. Among these, myxoid tumors and glomangiomas were completely removed through secondary resection and no recurrence occurred. One case of fibroma was diagnosed as clear cell sarcoma and was completely removed through secondary resection. One patient with fibroma was transferred to another hospital for a second opinion. None of the patients with malignant lesions developed systemic metastasis nor had its survival affected. Only one case of squamous cell carcinoma required additional treatment after wide excision. After radiotherapy, no recurrence was observed.
1. Clinical cases
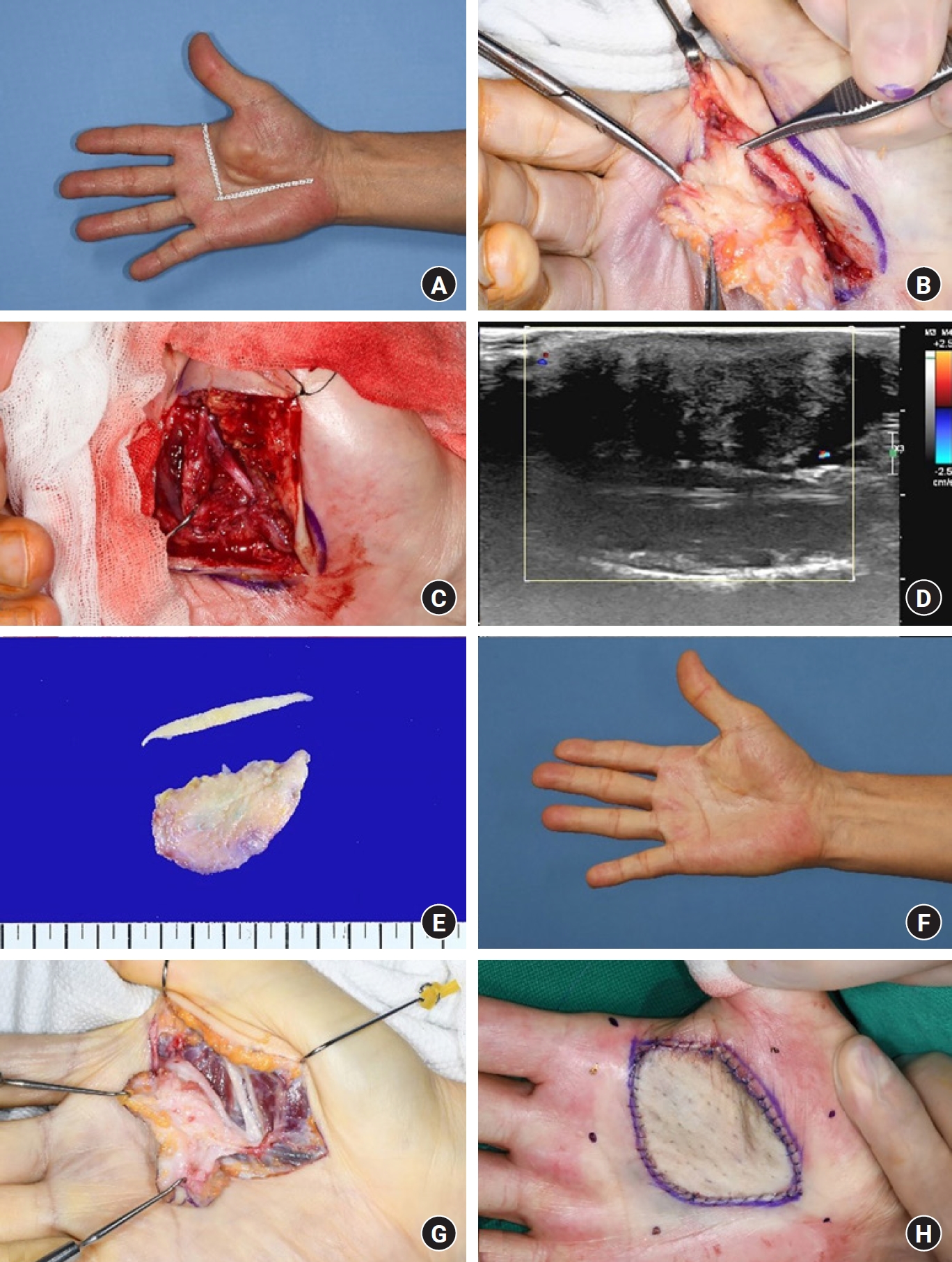
A 55-year-old male patient was admitted to our department with a cracked fingernail, swelling, and pain in the left index fingertip. A glomus tumor was clinically suspected owing to pain and nail lesions. USG revealed a well-defined homogeneous hypoechoic soft tissue mass of the medial aspect of the distal phalanx with prominent internal vascularity on color Doppler. Thus, we could reasonably suspect a glomus tumor. Excision was performed, including the nail, and pathological biopsy revealed fibroma. The wound healed without complications after 1 month. However, the mass recurred at the same location 1 year later, and re-excision was performed. A biopsy was performed and clear cell sarcoma was diagnosed. As the primary closure of the defect was impossible, a cross-finger flap was performed using the middle finger. After 3 weeks, flap detachment was performed, and the wound healed well without complications (Fig. 1).
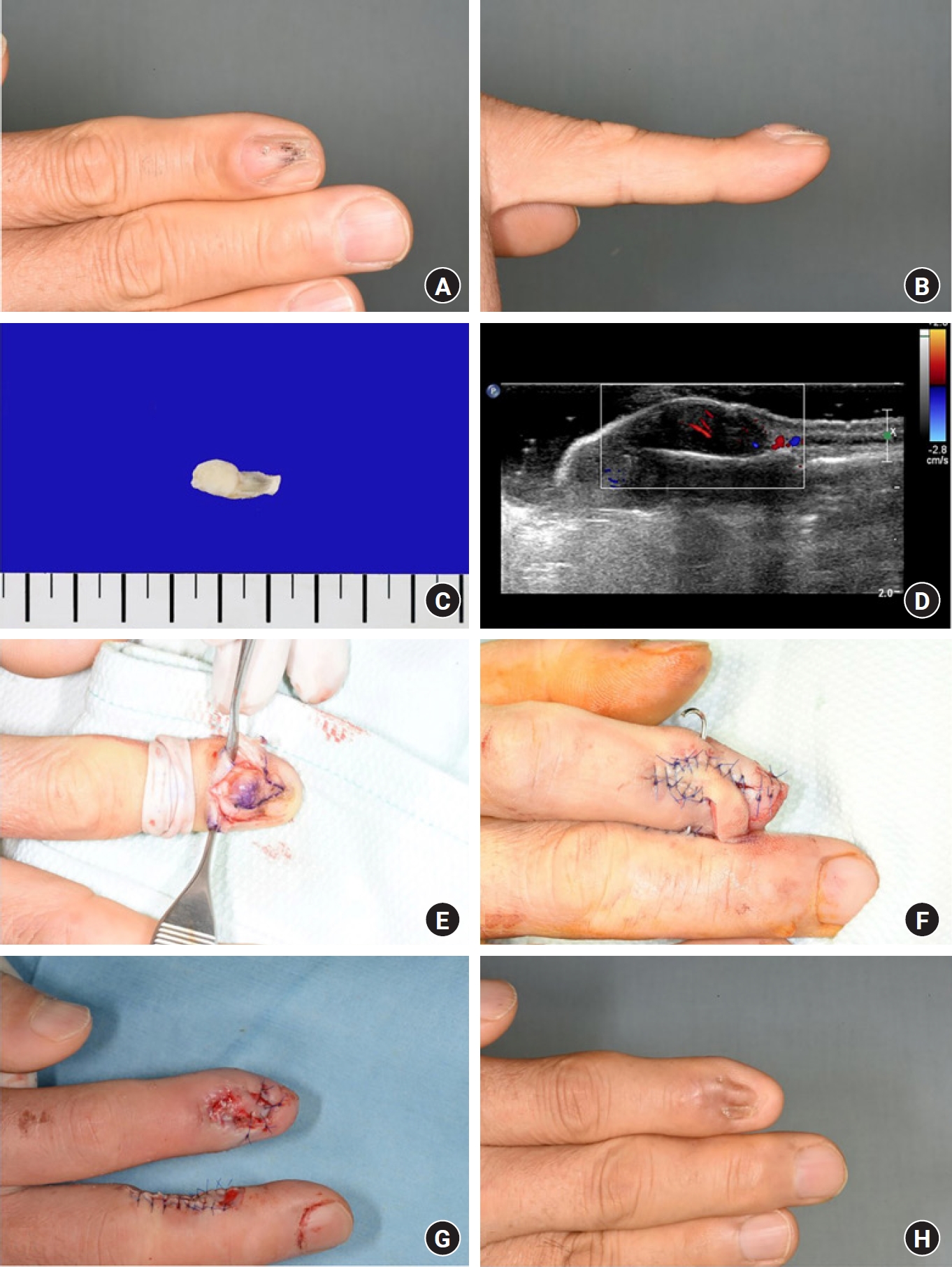
A 55-year-old man with a suspected glomus tumor underwent surgery; after the first operation, it was diagnosed as a fibroma. (A, B) Gross views of the finger lesion. (C) Postoperative biopsy. (D) The lesion was diagnosed as a suspected glomus tumor by a radiologist following preoperative ultrasonography. (E) The tumor recurred after 1 year. Following reexcision, it was diagnosed as clear cell sarcoma. (F) The defect was covered by a cross-finger flap. (G) After 3 weeks, flap detachment was performed. (H) After 6 months, the lesion had healed well, without complications.
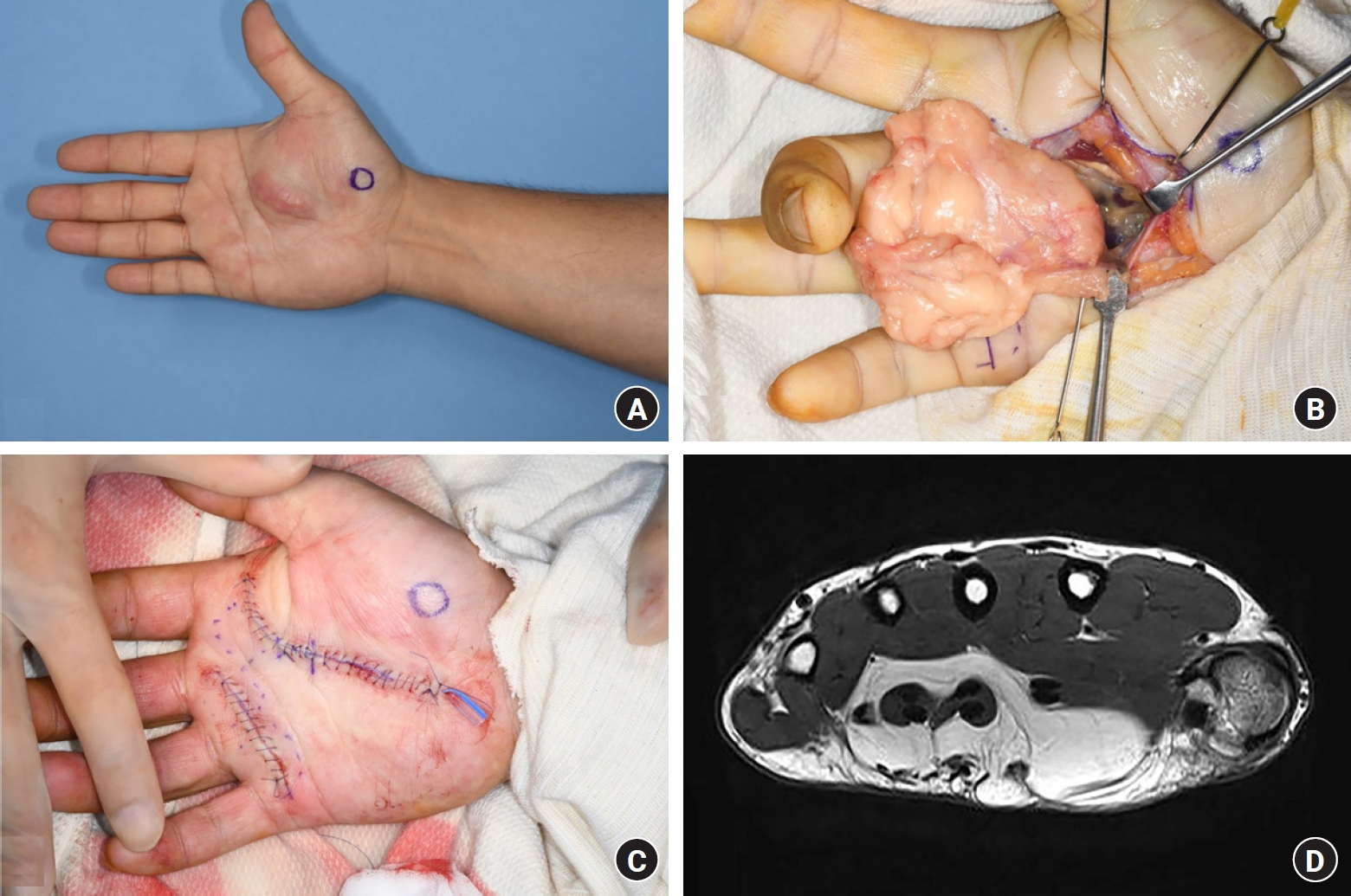
A 62-year-old male patient presented with swelling in the right thenar area that had been increasing for several years. Fibroma was clinically suspected because the lesion was hard and immobile. Preoperative USG revealed a lobulated heterogenous hypoechoic mass adhesive to the palmar fascia and thenar muscle; palmar fibromatosis was considered first. Most of the mass was removed during surgery, and a postoperative biopsy revealed it as a benign granular cell tumor. As the radial side of second common digital nerve was running through the tumor, the tumor was removed after cutting the nerve; subsequently, a neurorrhaphy was performed. After 1 year, the remnant tumor was excised and the defect was covered with a full-thickness skin graft. Although mild numbness of the fingers remained due to an injury, the symptoms gradually improved, and nerve regeneration progressed. The wound healed well (Fig. 2). After mass excision, the patient was able to resume manual tasks.
A 62-year-old man, suspected to have a fibroma, underwent surgery and was diagnosed with a granular cell tumor (benign). (A, B) Gross views of the palm lesion. (C) Fibrotic tissue was found, involving the common distal nerve to the index finger. Neurorrhaphy was performed following partial excision of the tumor. (D) The lesion was diagnosed as suspected fibromatosis by a radiologist following preoperative ultrasonography. (E) Postoperative biopsy. (F) After 1 year, a remnant mass was observed at the same site. (G) A secondary excision was performed. (H) The defect was covered by a full-thickness skin graft.
A 43-year-old male patient presented with swelling of the right thenar area. He underwent mass excision, but the mass rapidly regrew over several months. A lipoma was clinically suspected as the lesion was soft and movable. Preoperative MRI revealed an interval increased size of intramuscular fatty mass with septal internal enhancement in flexor digitorum muscles and tendons. An atypical lipoid tumor or a well-differentiated liposarcoma was suspected. The mass was removed without any complications, and a postoperative biopsy revealed a benign lipoma. The wound healed well (Fig. 3).
A 43-year-old man suspected to have a lipoid tumor underwent surgery and was diagnosed as having a benign lipoma. (A) A gross view of the palm lesion. (B) Mass excision was done. (C) Postoperative view. (D) The lesion was diagnosed as an atypical lipoid tumor or well-differentiated liposarcoma by a radiologist following preoperative magnetic resonance imaging.
Discussion
Few reports that provide a comprehensive analysis of hand tumors, including benign tumors, are available. Because not many tumors occur in the hand and the tumor types are variable, few studies have investigated hand tumors in Koreans. This study provides a better understanding of the frequency of hand tumors and the characteristics they present by analyzing each tumor. In particular, to the best of our knowledge, our research is the only one that has studied imaging modalities such as MRI and USG, which are frequently used for hand tumor diagnosis. We believe that surgeons treating hand tumors can avoid diagnostic errors with better knowledge.
In our study, ganglion cyst was the most common benign soft tissue tumor, followed by vascular anomalies. These findings are similar to previous studies that describe ganglion cysts as the most common benign soft tissue tumor [6-8]. We found that squamous cell carcinoma was the most common soft tissue malignant tumor and there was one case of chondrosarcoma as a malignant bone tumor in our study. Two previous studies also described squamous cell carcinoma as the most common tumor in hand [6,9]. The proportion of bone tumors in the hand showed various results (1.0% to 25.31%) for each paper, but in most cases, bone tumors were lower than soft tissue tumors [6,10,11]. Similarly, bone tumors in this study showed a rate of 6.2%.
To figure out the features of malignant tumor in hand, a Japanese study compared the characteristics of malignant and benign hand tumors and revealed that the probability of malignant tumors was significantly higher in patients with lesions larger than 1.9 cm in size or over 39 years of age [5]. We also found that patients diagnosed with malignant tumors were older than those diagnosed with benign tumors. However, we found that benign tumors were larger than malignant tumors in size. Similar to a previous study, malignant tumors showed recurrence and rapidly growing symptoms in our clinical experience. Therefore, rapid growth, change, progression of symptoms, and frequent recurrence (within 1 year) are characteristics of malignancy [12]. In the case of melanoma or chondrosarcoma, there are no remarkable features before they become large, so an accurate diagnosis in the early stage is important.
Preoperative imaging is essential for the accurate diagnosis of most hand tumors. Although history and physical examination alone can diagnose most of these lesions, additional imaging studies are needed to confirm the diagnosis or define the anatomic extension involved. As a result of our study, the diagnosis of ganglion cysts can generally be based on the clinical diagnosis, but both USG and MRI provided good support. We found no difference between the accuracy of the radiologic modalities; however, in the case of finger mass, the probability of misdiagnosis was higher than that of tumors located in other parts of the hand. Radiologists can make clear predictions regarding imaging tests, but discrepancies also exist. As observed in this study, 16.9% of the results were inconsistent between the imaging findings and the final pathological analysis. When the size of a lesion becomes smaller, such as the mass of a finger, several tumors presenting the same characteristics on MRI or USG are difficult to distinguish (e.g., glomus tumors and fibromas show low signal on T1-weighted MRI images); thus, the coincidence rate between image reading and the actual pathology seems to be lowered [7]. In this study, we considered that the concordance rate between image reading and pathological results was lower for lesions in the finger, as in these cases a significantly lower predictive rate than that for other sites was observed (p=0.04). Failure to suspect malignancy either radiologically or clinically can result in the delayed detection of malignancy. Therefore, for hand tumors, clinical characteristics, physical and pathological examination, including imaging, are all relevant factors, and a multidisciplinary approach is required.
Hand surgeons should consider several aspects when they encounter cases of hand tumors: accurate diagnosis, the anatomical structures around the tumor, hand functions, pain relief, but also the possibility of malignancy and a related systemic effect, and strategies to prevent tumor recurrence. Previous studies have shown that 68% of patients with sarcomas on the distal upper extremity had received previous treatment and that 95% of patients with sarcomas of the hands and feet were referred after previous treatment [13,14]. Our study had an average follow-up period of 6.98 weeks and a relatively low recurrence rate was found: there were four cases of recurrence, including only one case of recurrence as a sarcoma. When a malignant tumor is suspected radiologically or clinically, wide excision is always performed in our institution. Resection with an inadequate surgical margin results in a risk of 12 times higher of local recurrence, three times higher of metastasis, and five times higher death than that with an adequate margin [15]. Surgeons should have a better understanding of each tumor to perform the most adequate oncological treatment.
The present study had several limitations. First, this was a retrospective study, and we were limited by the information available in the medical records. Second, the number of patients was small. Third, only the reading considered the highest priority in the imaging modality was included in the study. A second likely reading was often available, but we did not consider it. This rigor may have resulted in the undervaluation of the radiological test. However, we found that malignant tumors showed no significant differences in size and age compared to benign tumors, and radiologic misdiagnosis was more frequent in finger tumors. We believe that these findings may provide general considerations for those who encounter hand tumors. Further studies with larger populations are required to investigate other radiologic modalities and distinct characteristics of malignant tumors.
Conclusion
We reviewed the cases of hand tumors over 20 years in Korean and demonstrated that ganglion cyst and epidermoid cyst were common benign soft tissue tumor, and squamous cell carcinoma was the most common malignant soft tissue tumor. We also found that bone tumor was less frequent than soft tissue tumors. Radiologic misdiagnosis was significantly frequent in finger tumors due to their small size. Thus, hand tumors, especially those suspected to be malignant, should be assessed using a multidisciplinary approach, including radiologic, clinical, and pathologic examinations.
Notes
The authors have nothing to disclose.
Funding
None.