The treatment of axillary hidradenitis suppurativa with a thoracodorsal artery perforator V-Y advancement flap: a case report
Article information
Abstract
Hidradenitis suppurativa, a recurrent and chronic inflammatory skin disease, presents with extensive scars and multiple abscesses. Moreover, axillary hidradenitis suppurativa could be impacted by scar contracture, which can limit arm mobility. The most reliable treatment for advanced hidradenitis suppurativa is meticulous and radical excision. Several methods exist for the reconstruction of axillary wounds after reconstruction. Skin grafts are an option, but their drawbacks include secondary contracture and poor aesthetic results. Local flaps could be useful, but also have a limited arc of rotation for larger defects. Thoracodorsal artery perforator (TDAP) flaps have been proven to be very effective as part of the armamentarium for axillary wounds. Herein, we describe the use of a TDAP flap in a V-Y advancement fashion with minimal pedicle dissection. We only dissected the perforator pedicle about 1 to 2 cm from its muscle entry point. With this maneuver, the flap could be easily moved to cover the defect without vascular compromise. We found that the TDAP flap performed in a V-Y fashion, with a propeller design, was very useful for an axillary defect over an island. This procedure was simple, easy, and time-saving.
Introduction
Hidradenitis suppurativa, which is a recurrent and chronic inflammatory disease affecting skin with apocrine glands, causes scars and abscesses in the affected skin and subcutaneous tissues. It often leads to odorous discharge, physical discomfort, and psychological distress in affected patients. The condition typically presents as scars, abscesses, nodules, and sinus tracts in areas such as the axilla, inframammary regions, buttocks, perineum, and groin. Conservative management has been employed to address initial symptoms, but its efficacy is limited, and the disease often recurs [1,2]. As a result, surgical excision of lesions is the preferred treatment for hidradenitis suppurativa to prevent recurrence [3,4]. The disease primarily impacts the axillary area, where scar tissue development and skin contraction can limit shoulder and arm mobility [5]. Skin grafts have several drawbacks, including lengthy rehabilitation, reduced range of motion due to secondary contracture, and unsatisfactory aesthetic and functional outcomes. Therefore, surgeons generally favor using flaps for coverage of the excised area. Local flaps sourced from the back provide high-quality skin, but their thickness can have negative aesthetic and functional consequences [6]. In this case report, the thoracodorsal artery perforator (TDAP) flap was used in a V-Y advancement fashion with minimal pedicle dissection. We only dissected the pedicle about 1 to 2 cm from the muscle entry point. With this maneuver, the flap was able to easily cover the defect without any vascular compromise. The procedure was simple, easy, and straightforward.
Case report
1. Patients
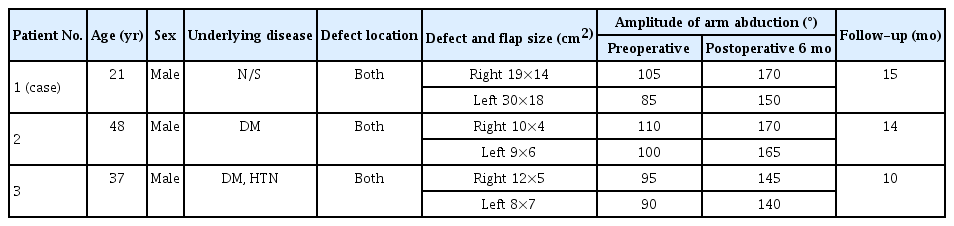
This study was conducted at the Department of Plastic and Reconstructive Surgery at Jeonbuk National University Hospital from April 2000 to December 2022. We discuss one case among three patients with severe hidradenitis suppurativa. All the patients underwent radical excision followed by immediate axillary reconstruction using a TDAP flap in V-Y advancement design. For the initial 2-week period, the shoulders were maintained at a 45° angle of abduction, while the elbows were kept flexed at 90°. Following this 14-day period, patients underwent controlled arm abduction and exercise supervised by an occupational therapist. The amplitude of arm abduction preoperatively and at 6 months after surgery was measured objectively using goniometry, which was performed in the frontal plane by an occupational therapist, with the patient standing and actively performing maximum arm abduction. The fixed part of the goniometer was positioned on the posterior axillary line and the moving part was positioned on the posterior arm, with its axis close to the acromion (Table 1).
The study was performed in accordance with the principles of the Declaration of Helsinki. It was approved for exemption by the Institutional Review Board of Jeonbuk National University Hospital (No. CUH 2023-03-029) and written informed consent was obtained from the patients for the publication of this report including all clinical images.
2. Surgical technique
Preoperatively, the TDAP was traced with a hand Doppler device (8 MHz, Bidop ES 100V3; Hadeco, Kawasaki, Japan) in a routine manner. The perforator originates from the descending branch of the thoracodorsal artery, roughly 8 to 13 cm from the axillary fold, and is situated about 0 to 5 cm from the anterior border of the latissimus dorsi muscle [7]. Based on the vascular anatomy outlined, a Doppler probe is utilized to locate the descending branch of the thoracodorsal artery, allowing for preoperative identification. The patient is positioned in a lateral decubitus posture with the respective upper arm abducted. Following palpation and marking of the front boundary of the latissimus dorsi muscle, the front extremity of the skin section is planned to be approximately 1 cm ahead of the anterior edge of the latissimus dorsi muscle. This strategic positioning is intended to ensure inclusion of the main perforators within the flap. A single V-Y advancement flap based on the marked musculocutaneous perforators of the thoracodorsal vessels was planned.
All hair-bearing skin in the axilla was excised down to the axillary vessels. After the radical excision of the lesion, V-Y flap harvesting began. First, the anterior skin was incised subfascially. Next, the superior border of the flap was elevated, followed by its posterior border. Once islanded, the flap was dissected subcutaneously until it was sufficiently mobile to close the primary defect. No additional effort was made to isolate the perforators, as the flap could be advanced comfortably. Once hemostasis was achieved, the flap was closed from below upwards, starting with the secondary defect. We gradually coaxed the flap into a diamond shape. The flap was then inset using subcutaneous and subcuticular absorbable sutures. After that, a negative pressure suction drain was applied, and the donor site was primarily repaired.
3. Case
A 21-year-old man presented to our department with hidradenitis suppurativa in both axillary areas. Symptoms had started about 5 years prior, and conservative treatment, including dressing and incision and drainage of abscesses, was performed for several years, but deterioration and improvement alternated. Two months before his visit, the symptoms severely worsened, with pus discharge and pain accompanying infection in the areas (Fig. 1). The patient had experienced psychological distress due to this condition for a long time, so he had also received psychiatric treatment, and he strongly wanted surgical treatment to prevent recurrence. Surgical excision of the affected tissue in both axillae was necessary, and reconstruction of the defects was inevitable.

Pus discharge and pain accompanying infection in both axillary areas. (A) Anterior view. (B) Right lateral view. (C) Left lateral view.
Since the lesions in both axillae were extensive, it was expected that the size of skin and soft tissue defects would be very large. Therefore, we planned to reconstruct the defects using a TDAP flap in a V-Y advancement design. The left axillary lesion was removed, and the defect size was quite large, at 30×18 cm. Since the defect size was substantial, the distal part of the defect underwent primary closure, reducing the defect size to 22×18 cm. The design of the flap took the size of the defect into consideration, starting from the area where the perforator was marked. The skin incision proceeded to the latissimus dorsi fascia and was carefully dissected from the anterior border of the flap. The skin flap containing the muscle strip was transferred to the defect in a tension-free manner, and the donor site was closed with primary closure. The defect size of the right axilla after removing the lesion was 19×14 cm, and the defect was reconstructed using the same method (Fig. 2).
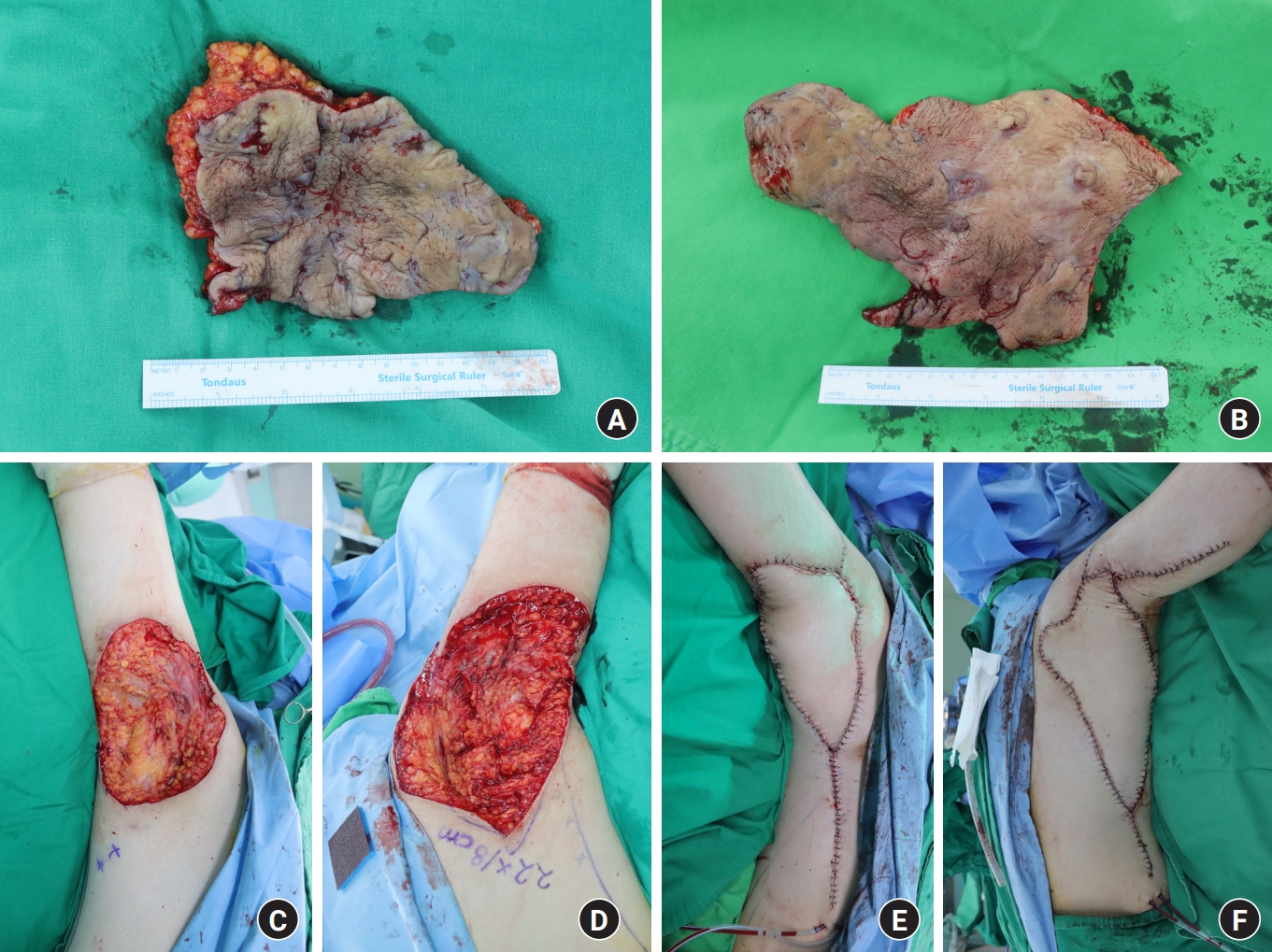
Intraoperative view. A thoracodorsal artery perforator flap in a 21-year-old man. (A) Excision of the affected tissue in the right axillary area. (B) Excision of the affected tissue in the left axillary area. (C) Skin and soft tissue defect in the right axillary area. (D) Skin and soft tissue defect in the left axillary area. (E) Immediate postoperative images in the right axillary area. (F) Immediate postoperative images in the left axillary area.
After surgery, the patient recovered well without any complications. At the 6-week follow-up, the patient carried on with daily life without difficulties (Fig. 3). The patient was successfully treated without any significant complications for 15 months.
Discussion
Hidradenitis suppurativa is a debilitating and chronic inflammatory disease affecting apocrine gland-bearing skin, with a prevalence of 1% to 4%. The disease is mostly hereditary, usually occurs after puberty, and has a higher prevalence in women and African Americans. Clinically, it presents as painful and recurrent hypertrophic scars, nodules, and abscesses in areas such as the perineum, gluteal cleft, inguinal folds, breast, and axilla. In severe cases, the disruption of normal skin structure interconnected sinus tracts and fistulae to form, along with extensive cutaneous and subcutaneous fibrosis. Several studies have investigated predisposing factors, and it is known that obesity and smoking exacerbate the severity of the disease [3].
In advanced axillary hidradenitis suppurativa, conservative treatment is generally ineffective; instead, radical surgical excision and axillary reconstruction are required. Considering our experiences and previous studies, local flaps have been preferred to skin grafts. Angrigiani et al. [8] published the first description of the TDAP flap. The TDAP flap can be brought to the axillary area via simple advancement, rotation, and displacement. Free mobility is a significant advantage compared to local flaps and random flaps that have restrictions in rotation because the vascular pedicle and base of the flap must be preserved [9].
The flap described in this case is a perforator flap utilizing the musculocutaneous branches of the thoracodorsal vessels to supply both the latissimus dorsi muscle and the skin covering it. In our specific case, we did not find it necessary to perform dissection down to the thoracodorsal vessels, as is typically done in a conventional TDAP flap, although this remains an option for larger defects. Baudet et al. [10] demonstrated that this system of vessels is highly reliable and easily identifiable, consistently present in all cases, and characterized by substantial vessel diameters. Angrigiani et al. [8] outlined the use of free perforator flaps based on the thoracodorsal artery, which enable the preservation of the latissimus dorsi muscle. Additionally, original cadaveric studies have shown that an axial-pattern fasciocutaneous flap can be harvested from one or two vessels originating as direct septocutaneous branches from the thoracodorsal vessels.
The TDAP flap offers several advantages due to the robust and predictable nature of the scapular-thoracodorsal arterial system. It is a reliable and reproducible flap option. By performing subfascial dissection, the fascial plexus can be preserved, allowing for a length-to-width ratio of 3:1. This preservation of the vascular system enables the flap to provide a large quadrilateral paddle of skin, making it suitable for closing large defects. Additionally, the procedure does not require immobilization of the shoulder, and the resulting scar can be easily concealed along the posterior axillary fold. The TDAP flap also offers excellent contour and texture matching, while preserving the natural axillary fold. Various designs of TDAP flaps can also be used, such as V-Y fashion, island, and propeller flaps. Each type of flap is powerful and robust and has its own advantages. However, the V-Y advancement flap has distinct merits compared to the island flap and propeller flap. It does not need extensive skeletonizing of the vessel and dissection of the surrounding area. Therefore, we can expect less vascular compromise and less tension when repairing the donor site.
We have not needed to include muscle in the flap or to dissect the perforators to close the axillary defects. This has resulted in a simpler and safer flap and we recommend its use in clinical practice for the treatment of axillary hidradenitis suppurativa.
Notes
The authors have nothing to disclose.
Funding
None.