|
 |
- Search
| Arch Hand Microsurg > Volume 28(3); 2023 > Article |
|
Abstract
Purpose
Infected malleolar bursitis sometimes requires multiple debridements, followed by soft tissue reconstruction with a flap. The purpose of this study was to evaluate the clinical outcomes of patients with infected lateral malleolar bursitis who were treated using peroneal artery perforator-based propeller flaps.
Methods
We retrospectively included 10 patients who underwent reconstruction of the lateral malleolus with a peroneal artery perforator-based propeller flap due to infected lateral malleolar bursitis between 2014 and 2022.
Results
The average follow-up time was 77.2 weeks. Six patients experienced complete healing; three developed partial flap necrosis, and one had a long-lasting seroma. All patients with complications had long-term diabetes.
Conclusion
Partial flap necrosis in patients with diabetes may occur because of impaired microcirculation. A peroneal artery perforator-based propeller flap could be useful for soft tissue reconstruction in select patients without diabetes or in patients with diabetes who have infected lateral malleolar bursitis.
Serial surgical debridement of infected bursa and peritendinous tissues might be needed to treat infected lateral malleolar bursitis. However, this procedure commonly results in a large dead space and loss of the soft tissue envelope in the lateral malleolus. After the infection is controlled to some extent, skin envelope coverage and filling of the dead space with a flap with a reliable vascular supply are necessary to achieve successful reconstruction.
Several flaps have been used to cover the soft tissue defect that results after debridement of infected lateral malleolar bursitis. Park et al. [1] and Kim et al. [2] have reported successful outcomes of reverse sural artery flaps in infected lateral bursitis. Infected lateral malleolar bursitis often occurs as a diabetic complication [2]. Although Kim et al. [2] reported successful outcomes of reverse sural artery flaps in diabetic patients with infected lateral bursitis, Parrett et al. [3] noted an increased risk of flap compromise and flap loss for reverse sural artery flaps in diabetic patients. The sacrifice of the sural nerve can be required for flap elevation and may cause permanent sensory loss of the lateral malleolus, which may encourage the recurrence of lateral malleolar bursitis [4]. Hashimoto et al. [5] reported a successful outcome of lateral calcaneal artery adipofascial flap in two patients with intractable infected lateral malleolar bursitis. However, as the flap is limited in size and does not have a skin flap, there is no possibility of tension-free skin closure at the lateral malleolus, which is located within the axis of rotation of the ankle joint [6].
The propeller perforator flap is a local island fasciocutaneous flap made of two paddles of unequal length that are separated by the nourishing perforating vessel forming the pivot point [7]. Because peroneal artery perforators were located adjacent to the lateral malleolus [8], peroneal artery perforator-based propeller flaps have been used for defects of the lateral malleolus [9]. Hong noted that although significant atherosclerotic changes are found in the major vessels of the lower leg in diabetic foot patients, perforating vessels, which are used as the vascular pedicle of propeller perforator flaps, are often spared from atherosclerosis [10]. Infected lateral malleolar bursitis often occurs as a diabetic complication [2]. Therefore, the propeller flap may be useful for treating intractable infected malleolar bursitis accompanied by diabetes. The purpose of this study was to evaluate the clinical outcomes of patients with infected lateral malleolar bursitis who were treated using peroneal artery perforator-based propeller flaps.
Ethics statement: The study was conducted after obtaining approval from the Institutional Review Board of Keimyung University Donsan Hospital (No. 2019-06-046). Written informed consent was obtained from the patients for the publication of this study, including all clinical images.
We retrospectively included all patients who underwent reconstruction of the lateral malleolus with a peroneal artery perforator-based propeller flap due to infected lateral malleolar bursitis between 2014 and 2022. All patients were referred to our department from the orthopedic department to cover a soft tissue defect after debridement of infected lateral malleolar bursitis. The patients had small- to medium-sized defects that were up to 16 cm2 in size, with peroneal tendon or bone exposure. The flap surgery was performed by one surgeon (JC). Medical charts were reviewed for demographic characteristics, preoperative factors (such as smoking status and comorbidities), operation time, and complications. On the final follow-up office visit, recurrence of bursitis was examined. Recurrence was defined as fluctuation and swelling in the lateral malleolus.
After general or spinal anesthesia was induced, a thigh tourniquet was applied to the leg without exsanguination to allow easier identification of the perforators during exploration. Perforating vessels branch from the peroneal artery and course through or near the posterolateral intermuscular septum of the lower extremity before reaching the subdermal plexus of the skin. Adjacent to the lateral malleolus, the peroneal perforators are located approximately 7, 5, and 3 cm from the tip of the lateral malleolus [8]. The flap was designed with respect to the defect. Under loupe magnification, an exploratory incision was made in one of the anterior margins of the flap design to confirm the targeted perforator. Perforator vessel patency was assessed with a handheld Doppler flowmeter both preoperatively and intraoperatively. After all boundaries of the flap were raised, we checked for fresh bleeding on all flap margins before flap rotation for at least 10 minutes. If the perforator vessel was reliable, all boundaries of the flap were raised with subfascial dissection. The septum surrounding the perforator was dissected to prevent kinking of the vessel when the flap was rotated. Once flap perfusion was verified after rotation, the flap was inset to the defect. In the case of a large extensive defect rather than a small opening, the de-epithelized distal portion of the flap was used to fill the dead space. If the donor site defect could not be closed primarily, a split-thickness skin graft was used to cover the defect.
Ten patients underwent reconstruction of the lateral malleolus for infected lateral malleolar bursitis (Table 1). All were male, with a mean age of 68 years (range, 55–79 years). Reconstruction was performed under general anesthesia in five cases and under spinal anesthesia in five cases. Of the 10 patients, seven had a smoking history, six were hypertensive, five were diabetic, and one was in chronic renal failure. The range of the duration of diabetes was from less than 1 to 30 years, with a median of 20 years. The mean HbA1c was 8.4% (range, 7.2%–9.8%). The mean duration of the operation was around 85 minutes. A single drain was typically positioned at the site of the flap during the procedure. The mean duration of drainage was 15 days. The average follow-up time after reconstruction was 77.2 weeks. Six cases achieved complete healing, while three developed partial flap necrosis, and one had a long-lasting seroma. In one patient, partial flap necrosis was resolved by secondary intention within 30 days. In two patients, the wound was treated with vacuum-assisted closure (VAC) followed by a split-thickness skin graft after three months of treatment. The patient with a long-lasting seroma was referred to the orthopedic department for closure of the fistula communicating with the ankle joint; the wound was treated with multiple debridements and VAC and resolved with secondary intention after 6 months of treatment. No patient experienced recurrence of bursitis during follow-up (Figs. 1-3).
Most cases of lateral malleolar bursitis can be treated conservatively, with methods such as aspiration, steroid injection, or compressive bandaging. If the conservative treatments are not effective, complete bursa resection and simple sutures can be applied [11]. However, infected malleolar bursitis is difficult to treat simply with bursa resection and requires multiple debridements and wound dressings over an extended period of time. Serial surgical debridement of infected bursa and peritendinous tissues commonly causes a large dead space and loss of the soft tissue envelope in the lateral malleolus. Therefore, in the final step of treatment of infected malleolar bursitis, the skin envelope must be covered and the dead space must be filled with a flap.
In our study, patients with infected lateral malleolar bursitis were treated using peroneal artery perforator-based propeller flaps. The complication rate was 40%, much higher than previous studies reporting usefulness of other flaps to treat infected lateral malleolar bursitis [2,5]. We assessed the reliability of the perforator vessel intraoperatively with a handheld Doppler flowmeter. We thoroughly dissected all fascial strands and soft tissues around the perforator to prevent kinking of the perforator vessel. In all cases with partial flap necrosis, flap congestion occurred in the distal portion of the flap and no total flap congestion was observed from the first day after the surgery. Despite efforts to resolve the congestion, the area experienced superficial or full-thickness necrosis. We checked for fresh bleeding on the distal flap margins intraoperatively, and the ratio of flap width to length did not exceed 1:4. Mehrotra [12] and Taeger et al. [13] noted that pedicled perforator flaps can be raised with width-length ratios up to 1:4.5 or 1:5. In our study, all partial flap necrosis occurred in diabetic patients. This may be due to impaired microcirculation [9]. Diabetes is known to lead to microvascular changes that can hamper flap microperfusion [14]. Impaired microcirculation may occur in the distal and less-vascularized portion of the flap through dysfunction of the linking vessels caused by microvascular injury in diabetic patients [15]. Therefore, the distal portion of our flaps might be affected by impaired microcirculation.
In two cases, a de-epithelized distal portion of the flap was used to fill the dead space. These patients had a large extensive defect rather than a small opening in the lateral malleolus. It is very important to prevent dead space in the lateral malleolus because of its location in the axis of rotation of the ankle joint [6], where seroma or hematoma may form after surgery. Lee et al. [16] noted that the dead space was reduced in patients with intractable lateral malleolar bursitis when using quilting sutures after bursectomy, preventing fluid collection and promoting wound healing.
One patient had a long-lasting seroma after surgery. This outcome may be because may have been caused by remaining infected bursa tissue or failure to close the fistula that communicated with the ankle joint. Lee et al. [16] reported usefulness of the intraoperative saline load test to find communication tracts between the bursal sac and the ankle joint. The intraoperative saline load test was very helpful to reduce postoperative seroma formation and recurrence of bursitis.
There are several limitations to our study. First, it was a retrospectively designed study. Second, it was a small-scale study. Despite these disadvantages, to the best of our knowledge, only two studies have reported soft tissue reconstruction using a flap after debridement of infected lateral malleolar bursitis [2,5]. Diabetic patients had a higher flap complication rate than nondiabetic patients. It is expected that a good surgical outcome can be obtained if the flap is selectively used in nondiabetic and mildly diabetic patients. Therefore, a peroneal artery perforator-based propeller flap could be useful for soft tissue reconstruction after debridement of infected lateral malleolar bursitis. In our study, 50% of patients had diabetes. Lateral malleolar bursitis develops as a result of repeated rubbing or pressure on the lateral malleolus. Hyposensitivity due to diabetic neuropathy may be one of the causes of bursitis. However, to the best of our knowledge, no prior study has reported a correlation between diabetic neuropathy and incidence of lateral malleolar bursitis. In the future, further examination into this correlation will be required to reduce the incidence of intractable infected malleolar bursitis in diabetic patients.
In our study, all partial flap necrosis cases occurred in diabetic patients. This may be a result of impaired microcirculation due to diabetes. A good surgical outcome would be expected if the flap is selectively used in nondiabetic and mildly diabetic patients. Therefore, a peroneal artery perforator-based propeller flap could be useful for soft tissue reconstruction after debridement of infected lateral malleolar bursitis.
Notes
Funding
This work was supported by Korea Nation Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (RS-2023-00240900).
Fig. 1.
A 73-year-old man with a 1×3 cm chronic wound on the lateral malleolus due to infective bursitis underwent treatment with a peroneal artery perforator-based propeller flap (A). (B) An intraoperative view. The arrowhead indicates the peroneal artery perforator. (C) Ten weeks postoperative.
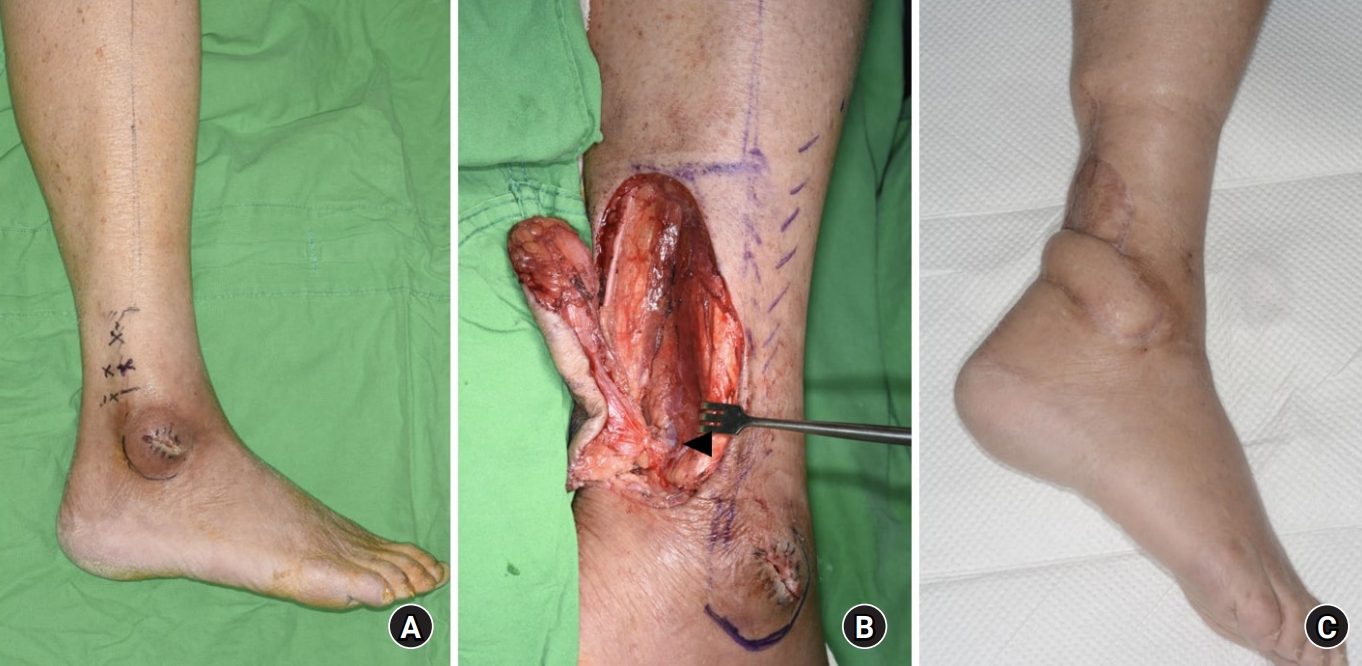
Fig. 2.
A 59-year-old man with a 3×2 cm chronic wound on the lateral malleolus due to infective bursitis underwent treatment with a peroneal artery perforator-based propeller flap (A). (B) Four weeks postoperative.

Fig. 3.
A 66-year-old man with a 3×2 cm chronic wound on the lateral malleolus due to infective bursitis underwent treatment with a peroneal artery perforator-based propeller flap (A). (B) Intraoperative view. (C) Three weeks postoperative: the necrotic process had progressed in the distal part of the flap.
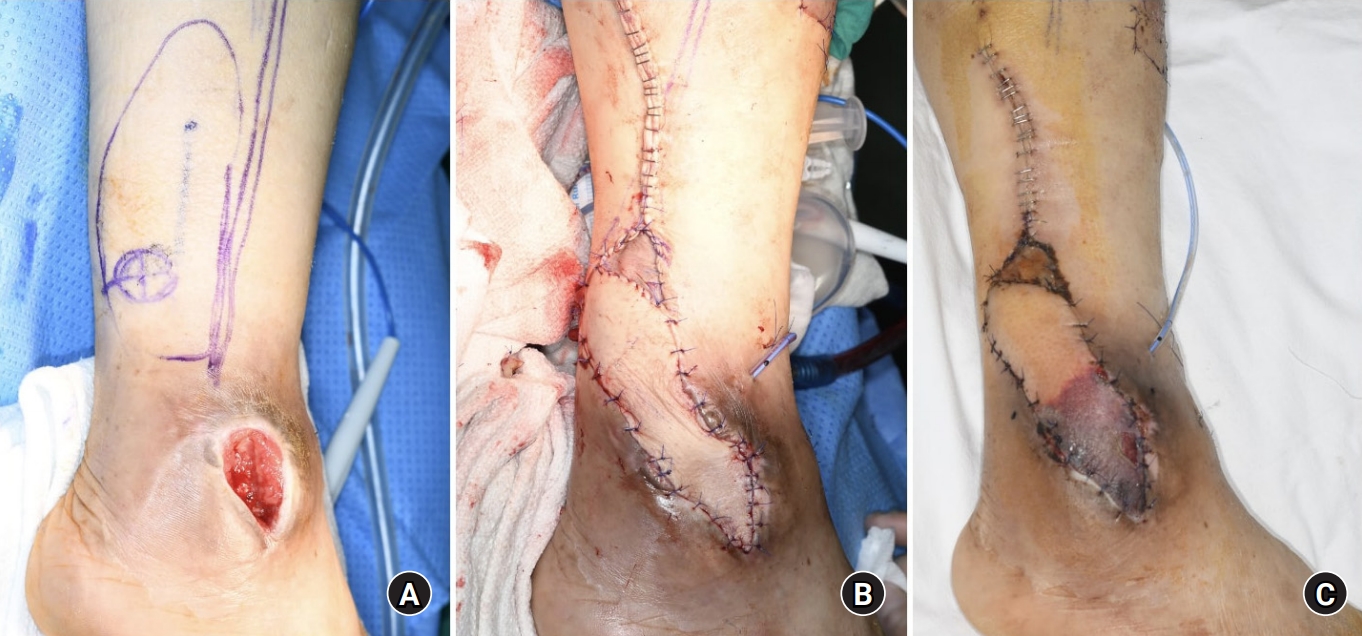
Table 1.
Patients’ summary
References
1. Park CH, Park JJ, Woo IH, Yan H, Lee WC. Characteristics of synovial fistula of the ankle joint: a case series. J Clin Med. 2022;11:6215.



2. Kim KJ, Ahn JT, Yoon KT, Lee JH. A comparison of fasciocutaneous and adipofascial methods in the reverse sural artery flap for treatment of diabetic infected lateral malleolar bursitis. J Orthop Surg (Hong Kong). 2019;27:2309499019828546.



3. Parrett BM, Pribaz JJ, Matros E, Przylecki W, Sampson CE, Orgill DP. Risk analysis for the reverse sural fasciocutaneous flap in distal leg reconstruction. Plast Reconstr Surg. 2009;123:1499-504.


4. Bamba R, Loewenstein SN, Adkinson JM. Donor site morbidity after sural nerve grafting: a systematic review. J Plast Reconstr Aesthet Surg. 2021;74:3055-60.


5. Hashimoto I, Yoshinaga R, Toda M, Nakanishi H. Intractable malleolar bursitis treated with lateral calcaneal artery adipofascial flap. Br J Plast Surg. 2003;56:701-3.


6. Barnett CH, Napier JR. The axis of rotation at the ankle joint in man: its influence upon the form of the talus and the mobility of the fibula. J Anat. 1952;86:1-9.


7. Pignatti M, Ogawa R, Hallock GG, et al. The "Tokyo" consensus on propeller flaps. Plast Reconstr Surg. 2011;127:716-22.


8. Mojallal A, Wong C, Shipkov C, et al. Vascular supply of the distally based superficial sural artery flap: surgical safe zones based on component analysis using three-dimensional computed tomographic angiography. Plast Reconstr Surg. 2010;126:1240-52.


9. Kim K, Kim J, Jeong W, Jo T, Park SW, Choi J. Outcome of distal lower leg reconstruction with the propeller perforator flap in diabetic patients. J Plast Surg Hand Surg. 2021;55:242-8.


10. Hong JP. The use of supermicrosurgery in lower extremity reconstruction: the next step in evolution. Plast Reconstr Surg. 2009;123:230-5.


11. Brown TD, Varney TE, Micheli LJ. Malleolar bursitis in figure skaters. Indications for operative and nonoperative treatment. Am J Sports Med. 2000;28:109-11.



12. Mehrotra S. Perforator-plus flaps: a new concept in traditional flap design. Plast Reconstr Surg. 2007;119:590-8.


13. Taeger CD, Horch RE, Dragu A, Beier JP, Kneser U. Perforator flaps. A new era in reconstructive surgery. Chirurg. 2012;83:163-71.



14. Eren S, Rübben A, Krein R, Larkin G, Hettich R. Assessment of microcirculation of an axial skin flap using indocyanine green fluorescence angiography. Plast Reconstr Surg. 1995;96:1636-49.