|
 |
- Search
| Arch Hand Microsurg > Volume 28(1); 2023 > Article |
|
Abstract
Swan neck deformity is characterized by hyperextension of the proximal interphalangeal joint and limited extension of the distal interphalangeal joint, showing the shape of a swan’s neck. The deformity can occur either acutely or chronically. A common acute cause of this deformity is trauma, and a common chronic cause is a secondary deformity due to rheumatoid arthritis. The treatment of swan neck deformity tends to depend on the knowledge and experience of the physician because the number of cases that hand surgeons can experience is limited, and there are no clear guidelines on treatment options. This review introduces the known causes of swan neck deformity and its treatment options. For swan neck deformity, the cause of the deformity, the elapsed time, the stage of the deformity, the biomechanical relationship between adjacent joints, and the functional limitations and needs of the patients must be considered when determining the treatment method. Based on these considerations, an appropriate choice should be made between nonsurgical and surgical treatment. The patients should receive a full explanation before treatment that an optimal outcome is not always guaranteed. The treatment process requires full understanding and cooperation from the patient.
손가락의 신전-굴곡 기전은 다양한 근육과 건들로 이루어진 복잡한 구조로, 조정하는 힘의 균형이 무너질 경우 백조목 변형 또는 단추구멍 변형과 같은 손가락의 변형이 발생하게 된다[1]. 변형들은 급성 또는 만성으로 발생할 수 있으며, 급성은 외상에 의한 것이 가장 일반적이고 만성으로는 류마티스 관절염에 의한 이차적인 변형이 흔하다[2,3]. 백조목 변형이 단추구멍 변형보다 빈번하게 발생하는 것으로 알려져 있다[2]. 백조목 변형은 특징적으로 근위 지관절(proximal interphalangeal joint)의 과신전 및 원위 지관절(distal interphalangeal joint)에서의 신전 지연으로 백조의 목과 같은 형상을 보이는데, 환자는 이로 인한 미용적인 문제와 기능적 장애를 호소한다(Fig. 1). 특히 주머니에 손을 넣거나 장갑을 낄 때 굴곡된 원위 지관절에 방해를 받고, 수지 굴곡 시 과신전된 근위 지관절이 한 번에 자연스럽게 굴곡되지 않고 두 단계에 걸쳐 굴곡되는 현상이 발생하여 환자가 물건을 쥐기 어려워지므로 불편함을 느낀다.
백조목 변형은 수부외과 의사가 경험할 수 있는 증례가 제한적이고, 현재까지도 치료 방법에 대한 명확한 지침이 없어 치료하는 의사의 지식과 경험에 의존하는 경향이 있다. 또한 구조적으로 인대 유연성(ligamentous laxity)을 가진 환자에서 정상 생리적으로도 백조목 변형이 보이는 경우도 고려해야 한다. 마지막으로 변형을 발생시키는 원인이 다양하고 근위 지관절 이외 인접 관절의 문제로도 변형이 발생할 수 있기 때문에, 치료를 결정하기 전 이러한 모든 요소들을 정확히 파악하여 적절한 치료 대상과 방법을 선택하여야 좋은 결과를 기대할 수 있다. 그럼에도 항상 최선의 결과가 보장되는 것은 아니며, 불량한 결과를 보이기도 한다. 본 종설에서는 지금까지 알려진 백조목 변형의 원인들과 그 치료법들에 대해 고찰하고자 한다.
수지 신전-굴곡 기전의 해부학을 이해하는 것이 백조목 치료에 매우 중요하다. 수지의 신전은 수장측의 굴곡건에 대항적으로 작용하며, 외재근에 해당하는 수지 신전건(extensor digitorum communis)은 중수지 지관절의 신전을 담당한다. 내재근에 해당하는 충양근(lumbrical muscle) 배측 및 장측 골간근(dorsal and volar interosseous muscle)은 수지 신전건에 대항하여 중수지 지관절 굴곡 역할을 하지만, 근위지 및 원위지 관절에서는 신전을 기능한다. 이러한 수지의 굴곡과 신전은 다양한 근육의 복합적인 작용으로 발생하는데, 균형 잡힌 수지 운동의 중요한 요소는 굴곡건 및 신전건의 해부학적 길이를 유지하는 것이며, 해당 건을 해부학적 위치에서 안정적으로 잡아주는 다양한 인대의 역할 역시 중요하다.
정상적인 신전건의 excursion은 굴곡건에 비해 작으며, 근위에서 원위로 갈수록 그 크기가 줄어든다. 문헌에 따르면 각 관절을 신전시키기 위해 필요한 해당 신전건의 excursion은 중수지 관절의 경우 5 mm, 근위 지관절은 4 mm, 원위지 지관절은 1–2 mm 정도이다[4].
수지 신전건은 근위지골의 배측을 지나며 가운데 중앙 신전건과 양측의 측부대로 총 세 가닥으로 나뉘게 된다. 중앙 신전건은 중위지골 기저부 배측에 붙어 주행하며, 근위 지관절에 닿는 곳 부근에서 내재건의 일부와 합쳐져 central band를 형성하며 근위 지관절의 신전을 담당한다. 측부대는 충양근과 배측 골간근과 합쳐지며 윈위부로 주행하여 병합 측부대(conjoined lateral band)가 되며 두 가닥의 병합 측부대가 중앙에서 다시 합쳐지며 종말 신전건(ternminal extensor tendon)을 형성한다. 종말 신전건은 원위지골 기저부에 붙어 원위 지관절의 신전을 담당한다(Fig. 1) [5].
나선빗인대(oblique retinacular ligament)와 가로빗인대(transverse retinacular ligament)는 정확한 기능에 대해 논란의 여지가 있는 구조물들이지만, 최근 연구들에서는 근위지 관절과 원위지 관절의 움직임을 동기화해 주는 것으로 보고되었다[6]. 나선빗인대는 원위부로는 종말 신전건에 부착하고 근위부로는 수장측 굴곡건막에 부착한다. 즉, 원위지 관절에서는 배측을 지나고 근위지 관절에서는 수장측을 지나기 때문에, 근위지 관절이 신전할 때의 장력을 종말 신전건에 전달하여 원위지 관절이 동시에 함께 신전되도록 도와준다. 전체 인구의 약 40%–50%에서만 기능한다는 보고도 있다[7]. 가로빗인대는 근위지 관절의 양측에 있는 굴곡건막에서 시작하여 병합 측부대의 양측 경계에서 끝난다. 근위지 관절이 굴곡하면 병합 측부대를 수장측으로 당겨 원위지 관절이 함께 굴곡되게 해주고, 근위지 관절이 신전할 때는 측부대의 배측 전위를 막는 역할을 한다. 삼각인대(triangular ligament)는 중위지골 원위부에 위치하며 나선빗인대와 가로빗인대의 반대작용을 하는 인대로, 병합 측부대를 배측으로 유지하게 해준다(Fig. 2). 손상을 받을 경우 측부대의 수장측 아탈구가 일어나 단추구멍 변형의 원인이 될 수 있다[5,8].
백조목 변형은 근위지 관절 자체의 문제로 발생할 수 있지만, 중수지 관절(metacarpophalangeal joint), 원위 지관절, 심지어는 손목 관절에서도 특정한 원인으로 시작되어 2차적으로 발생할 수 있다. 변형을 유발하는 원인은 외상에 의한 경우가 많으며, 질환의 경우 류마티스 관절염, 소아마비가 흔한 것으로 알려져 있다[2,3]. 변형의 시작 위치와 원인이 다양하여 이에 대한 파악이 변형을 파악하는 데 중요한 요소이다.
1979년 Zancolli 등[9]은 외상에 의한 백조목 변형을 근위 지관절을 중심으로 외인성 원인, 내인성 원인, 관절 내 원인의 세 가지 카테고리로 분류하였다. 외인성 원인으로는 망치 수지, 손목 관절, 또는 중수지 관절의 굴곡 구축이 포함되며, 내인성 원인으로는 만성적인 중수지 관절의 수장측 탈구, 허혈성 구축, 건 유착이 있다. 관절 내 요인으로는 천수지굴건(flexor digitorum superficialis) 손상과 수장판(volar plate) 손상이 있다(Table 1) [9].
외인성 원인으로는, 중수지골에 과도한 신전력이 가해지면서 백조목 변형이 시작된다. 예를 들어, 망치 수지 손상에서 말단 신전건이 손상되면 원위 지관절이 굴곡되고 측부대(lateral band)가 근위부 및 배측으로 이동하면서 중수지골이 과신전하게 된다. 대조적으로 손목 관절이나 중수지 관절의 굴곡 구축에서는 굴곡 구축에 대항하기 위해 수지 신전건의 장력이 증가하게 되고 수지신건은 중수지골의 배측에 부착하기 때문에 중수지골이 과신전하게 된다.
내인성 원인에서는 내인근들의 구축(intrinsic tightness)으로 인하여 변형이 발생하게 된다. 구획증후군이나 압궤 손상에 따른 허혈성 구축이 대표적이며 만성적인 중수지 관절의 수장측 탈구에서도 마찬가지로 내인근 구축이 일어난다.
피노키에토-번넬 검사(Finochietto-Bunnell test)가 내인근 구축을 확인하기에 유용하다[10]. 정상적으로 중수지 관절의 신전은 근위지 관절의 운동에 제한을 주지 않는데, 내인근 구축이 있는 경우에는 영향을 받게 된다. 중수지 관절을 완전히 편 상태와 완전히 구부린 상태에서 근위지 관절을 수동적으로 최대 굴곡할 수 있는 각도가 달라지면, 즉 중수지 관절을 구부린 상태에서 근위지 관절의 굴곡 범위가 증가한다면 검사 양성이며 내재근 구축을 시사하는 소견이다(Fig. 3). 근위지 관절의 굴곡 범위가 같다면 다른 원인들, 특히 관절 내 원인들을 감별하여야 한다.
관절 내 원인으로는 근위지 관절 수장측에서 기원한 원인들로, 수장판이 손상되어 만성적으로 이완될 경우(volar plate laxity) 근위지 관절의 수장측 탈구와 과신전이 일어나게 된다. 천수지굴건 역시 근위지 관절의 수장측에서 지지대(stabilizer)로 작용하기에 천수지굴건이 손상될 경우 역시 백조목 변형이 일어나게 된다.
백조목 변형의 치료는 유발 원인과 위치에 따라 다양하며, 치료를 시작하기 전에 이환기간과 환자의 불편한 증상, 그리고 관절의 파괴 정도를 반드시 함께 고려해야 한다. 자세한 문진을 통하여 이전에 있었을지 모를 수상력과 함께 기저질환에 대한 파악이 선행되어야 하고, 건측 수지와 항상 비교하여 인대 유연성의 소지가 있는지 파악하여야 한다. 인대 유연성을 가진 사람 중에는 외형적 변화는 있을지언정 기능적 문제나 불편함은 없거나 경미한 사람들이 있으므로 치료의 대상인지 신중하게 판단하여야 한다. 또한 치료 방침을 세울 때 유발한 원인뿐만 아니라 증상의 지속 기간, 불편함의 정도, 관절의 상태 등을 종합적으로 고려해야 한다. 이학적 검사는 이웃한 다른 관절들을 함께 평가하여야 하며, 앞서 언급한 피노키에토-번넬 검사를 포함하여 수동 및 능동 관절 가동범위, 동반 변형 유무 등을 함께 파악하여야 한다. 백조목 변형은 기능적 결함이 크지 않고 치료를 하더라도 항상 최선의 결과를 보장하는 것이 아니기 때문에 치료를 시작하기 전에 환자와 충분한 상의를 거쳐야 한다. 수술적 치료 역시 관절 가동범위 자체를 증가시키는 것이 아니라 휴식 상태의 신전 위치를 증대하여 물건을 잡는 동작을 쉽게 만드는 데 목적이 있다.
언급한 바와 같이 백조목 변형은 기능적 결함이 적고 적극적으로 치료하더라도 만족스러운 결과를 얻지 못할 우려가 있어, 일상생활에 적응하며 경과를 관찰하는 것도 방법 중 하나일 것이다. 이동성이 있는 백조목 변형, 근위 지관절의 가동범위가 정상이며 경증의 변형을 가진 Nalebuff 분류 1, 2단계 환자들에서 제한적으로 적용할 수 있다. 비수술적 치료의 방법으로 8자형 부목이나 신전 제한 부목을 사용할 수 있다[12,13]. 8자형 부목들은 삼점(3-point) 고정을 통하여 근위 지관절의 과신전을 방지하고 내재근의 구축을 막아준다. 신전 제한 부목은 근위지 관절의 과신전을 막아 기능적으로 근위지 관절 굴곡이 시작되기 더 쉽게 해준다. 이러한 부목들은 환자의 협조가 치료에 큰 영향을 미치는 것으로 알려져 있고, 종일 착용이 권고되기 때문에 피부 자극이나 이상 감각 등이 부작용으로 나타날 수 있다[12,13]. 특히 류마티스 환자들은 뼈의 돌출된 부분에 피부 자극이 되지 않도록 신경 써야 한다. 내재근 구축을 막기 위한 수동적 스트레칭을 포함한 관절 가동범위 회복 치료가 도움된다는 보고도 있으나 적용이 제한적이다[13].
다양한 수술적 치료를 크게 3가지 카테고리로 구분하는데, 망치 수지에 의한 이차적 백조목 변형에서 시행되는 신전-굴곡 기전 재조정 술기(extensor mechanism rebalancing), 근위지 관절의 과신전을 막아주는 근위지 관절 수장측 봉합술(volar tenodesis), 그리고 원위지 관절과 근위지 관절에 걸쳐 영향을 미치는 새로운 인대를 만드는 재건술(oblique retinaculum ligament reconstruction)을 큰 범주로 볼 수 있고, 각각의 범주는 세부적인 술식을 포함한다. 본 종설에서는 술식을 시행하는 위치에 따라서 각 세부적인 술식을 서술하였다.
외인성 원인 중 망치 수지로 인해 원위 지관절의 변형만 있는 경우는 엄밀하게 정의하자면 백조목 변형 상태는 아니지만, 적절하게 치료받지 않은 만성 망치 수지나 일차 치료가 실패한 경우 백조목 변형으로 진행하게 되어 수술적 치료가 필요하며 관절 상태에 따라 건피부 고정술 또는 관절 유합술을 시행할 수 있다.
건피부 고정술은 파열되고 늘어난 종말 신전건을 흉터화된 건 조직을 제거한 뒤 직접 피부와 함께 봉합하는 술식이다[14]. 관절 간격이 유지된 상태에서 적응증이 되며, 통상 원위 지관절 배측 방추형의 작도를 하고 피부를 포함하여 늘어난 건 및 흉터 조직을 같이 절제한다. 종말건의 혈행을 보존하기 위해 건을 피부와 박리하지 않은 채로 수직 끝맞춤 봉합법(vertical mattress suture)를 사용하여 2–3 mm 정도 종말건을 중첩하여 봉합하며, 원위 지관절을 최대 신전 상태로 유지하기 위해 커슈너 강선(Kirschner wire, K-wire)과 함께 고정한다. K-wire는 약 8주간 유지 후 제거하며 본 술식으로 10° 미만의 신전 지연을 보인 좋은 결과들이 보고되었다[14,15]. 경우에 따라서는 배측 골 돌기(osteophyte)를 같이 제거하기도 하며, 절제된 신전건과 피부를 따로 봉합하기도 한다(Fig. 4). 최근에는 종말건을 강화하기 위해 탈상피화 유경 피부 피판술(deepithelialized pedicled skin flap technique)을 병행하여 좋은 결과를 보고하기도 하였다[16].
근위 지관절의 변형을 치료하기 위한 수술적 방법으로 중앙건 절제술, 수장판 중접술, 천수지굴건 고정술 등이 있다. 이런 술기들은 원위지 관절의 신전 기전을 회복시킬 수는 없지만, 그 공통적인 목표는 근위지 관절의 과신전을 막는 것이다. 2017년 Kiziridis과 Giddins는[20] 메타 분석을 통하여 백조목 변형의 근위지 관절 변형에서 적용할 수 있는 연부조직 술기 중 최적의 술기를 알아보고자 시도하였으나, 각각의 장단점들이 뚜렷하여 결론을 내지 못하였다.
오랜 기간 변형이 지속되거나 Nalebuff 단계 3 이상으로 근위 지관절 배측의 피부 구축이 발생한 경우는 추가적인 피부 이식술 또는 Z-성형술 등이 필요할 수 있다. 수장측 술기만으로 부족할 경우 배측 관절낭 유리술이 근위 지관절의 과신전을 해결하는 데 도움이 된다[11].
무언가를 새로 절제해서 변형을 치료한다는 개념은 얼핏 보면 생소하지만, 백조목 변형이 신전-굴곡 기전의 불균형으로 나타난다는 점을 생각할 때 중앙건 절제술은 신전-굴곡 기전을 재정렬시키는 방법으로 이해할 수 있다[21]. 중앙건을 통해 근위 지관절에 과도한 신전력이 전달되고 있는 상태에서 절제술을 시행하면 측부대로 힘이 분산되며 종말 신전건까지 전달되어 원위 지관절의 신전에도 도움이 된다[22,23].
중앙건 절제술은 신전건의 연속성이 유지되고 원위지 관절의 신전 지연이 40° 미만인 경우 적응증이 된다. Fowler 술식으로 알려진 배측 종절개를 통해 근위 지관절 위쪽의 건에 접근할 수 있으며, 근위지 관절로부터 5 mm 근위부에서 중앙건 폭의 50%를 절제할 것이 권고된다[24]. Rozmaryn [24]은 중등도의 만성 추지 변형에서 중앙건 절제술과 원위 지관절 신전건 봉합 수술을 동시에 시행하여 좋은 결과를 보고하기도 하였다. 중앙건 절제 수술 중 측부대와 삼각인대(triangular ligament)가 손상되면 역으로 단추구멍 변형을 만들 수 있으므로 수술 중에 유의하여야 한다. 그럼에도 지금까지 보고된 임상 결과들을 보면 만성 망치 수지에 의한 백조목 변형을 본 술식으로 10° 미만의 신전 지연만 남도록 교정할 수 있었다는 보고들이 다수 있으며, 다만 초기 근위 지관절의 과신전이 25°를 넘는 경우에는 결과가 좋지 않아 사형지대 재건술을 시행할 것을 권유하였다[22,23,25,26].
만성적인 수장판 손상에 의해 백조목 변형이 생긴 경우, 수장판의 장력을 강화하기 위해 수장판 중첩술을 시행할 수 있다. 1980년 Eaton과 Malerich 등[27]에 의해 수장판을 근위 지관절을 통과하여 배측에 봉합하는 수장판 성형술(volar plate arthroplasty)이 보고된 이후로 다양한 술기와 기구를 이용한 수장판 중첩술이 시도되었다[27]. 중위지골 표면에 새로운 도랑을 만드는 방법, 골내 터널을 이용한 풀아웃(pull-out) 방법 등 다양한 수술적 방법이 보고되었으며, 본 저자들은 2 mm 이하의 작은 anchor를 사용하여 수장판을 중첩하는 방법을 선호한다(Fig. 5). 백조목 변형에 한정하여 수장판 중첩술만을 시행한 보고는 없으며, 54예의 만성적인 수장판 손상을 수장판 중첩술로 치료한 연구에서 7명이 백조목 변형을 초기에 확인하였고 수술 이후 모두 호전되었다고 보고한 연구가 있었다[28]. 백조목 변형을 교정하기 위한 다른 술식들의 발전으로, 수장판 손상이 없는 백조목 변형에 대한 수장판 중첩술의 단독 시행은 드문 추세이다.
천수지굴건은 수장판과 함께 수장측 지지대 역할을 하기 때문에 천수지굴건 고정술을 통해 백조목 변형의 호전을 기대할 수 있다. 1975년 Nalebuff와 Millender [29], 1980년 Curtis [30] 등이 처음 소개하였으며, Bruner 절개를 통한 수장측 접근을 하며 천수지굴건의 한쪽 가닥을 A2 활차 또는 굴곡건 건막에 봉합하여 고정하는 술식이다(Fig. 6). 이후 1986년도에 천수지굴건의 척측 가닥을 절반으로 나누어 절반만 골에 고정하는 식의 변형이 소개되었다(Fig. 7) [31]. 필요 시 suture anchor를 통해 수장판 중첩술을 함께 시행할 수 있다. 천수지굴건 고정술은 신전 기전에 영향을 주지 않는다는 장점이 있으나 원위지 관절의 변형까지 한 번에 교정하기는 어렵다. 따라서 원위지 관절의 변형이 심하지 않은 경우에 적응증이 된다[32]. 잠재적인 굴곡건 근력 감소와 A2 활차까지 함께 이환되어 늘어나 있을 경우 시행하기 어렵다는 단점이 있다[32]. 수장판 중첩술과 마찬가지로 단독 시행을 통해 임상적 결과를 보고한 논문은 많지 않다. 최근 연구 결과에서 수장판 중첩술과 천수지굴건 고정술을 비교한 종설이 있었으나 두 술식 간의 임상적 차이는 발견하지 못하였다[33]. 외상 후 발생한 백조목 변형 12예를 치료한 보고[34]와 류마티스 관절염에 의한 백조목 변형 23예를 치료한 보고[35]가 있다. 수술 후 근위지 관절 굴곡 구축이 발생하거나 신전 지연이 잔존하는 경우 예후가 불량하다.
1966년 Littler [36]에 의해 처음 소개되었으며, 측부대를 절단하여 수장판과 굴곡건 사이의 굴곡건막에 봉합하는 술식이다. 측부대의 연속성을 유지한 채로 수장측으로 지나는 방향을 바꿔주는 술기이다[36]. 류마티스 관절염에서 동반되는 손가락의 척측 변위를 줄이기 위하여 척측 측부대를 사용하는 방식의 수정을 거쳐, 척측 측부대를 거상시켜 굴곡건 A3 활차에 고정하는 술식으로 발전하였다[9,37]. 수정을 가한 사람들의 이름을 붙여 Zancolli-Tonkin 술식으로 불리우기도 한다. 다양한 원인의 백조목 변형에 모두 적용할 수 있으며, 측부대를 이용하기 때문에 원위지 관절까지 변형을 교정하는 효과를 줄 수 있다는 장점이 있다. 많은 수의 연구들이 양호한 결과를 보고하였다[37-39].
Littler [36]가 1966년 처음 발표한 뒤로 1978년 Thompson 등[40]이 발전시킨 방법이다. 자유 건 이식편을 사용하여 인위적인 건고정을 만들어주는 술식으로, 40° 이상의 신전 지연에 적응증이 될 수 있다. 본 술식으로 근위지 관절의 굴곡과 원위지 관절의 신전의 향상을 동시에 기대할 수 있는데, 측부대를 이용한 보고도 있으나 주로 장장근을 사용한 자유 건 이식편이 사용되어 왔다[41]. 본 술식은 일종의 동적 건고정술로 근위지 관절이 능동적으로 신전될 때 원위지골 기저부에서 근위지골까지 위치시킨 인대가 원위지 관절의 수동적 신전을 도와주어 원위지 관절도 동시에 같이 신전되도록 해준다. 중수지골 수장측부터 원위지골의 배측까지 새로운 인대를 재건하게 되며 양측은 풀아웃 방식이나 봉합나사로 고정한다(Fig. 8). 고정방식에 따른 결과 차이는 없는 것으로 보고되었다[41,42].
번넬 검사 양성 소견인 백조목 변형들, 즉 내재근의 구축이 있을 경우에는 내재근 유리술이 도움이 될 수 있다[44]. 원위지 관절과 마찬가지로 근위지 관절에서도 심한 관절염 진행이 동반된 경우 인공관절 치환술 또는 관절 유합술을 구제술식으로 고려해 볼 수 있다. 인공관절 치환술의 경우 본 종설의 범위를 넘어선다.
내재근 유리술은 강직성 소아마비 환자에서 근위지 관절 구축이 20° 이상이며 번넬 검사 양성인 경우 적응증이 된다[44]. 수술적 기법으로 원위 손바닥 주름(distal palma crease)을 따라 손바닥을 가로지르는 수평 절개를 통하여 모든 수지의 내재근에 접근할 수 있다. 신경혈관 다발을 피해 충양근에 도달하여 근육-건 경계부에서 부분적으로 유리술을 시행한다. 유리술은 건마다 2회씩 시행하며, 모든 과정이 끝난 뒤 번넬 검사를 재시행하여 호전 정도를 평가한다. 과하게 유리된 경우 굴곡건 근력 감소가 일어날 수 있어 유의하여야 한다.
류마티스 관절염 환자의 90% 정도가 손의 변형을 겪는 것으로 알려졌으며 백조목 변형은 이런 변형 중 가장 흔하다[11]. 이러한 변형들은 류마티스 관절염 초기부터 발생할 수 있으며, 질병 활성도의 예측인자로도 사용되기도 한다[45]. 또한 환자의 일상생활 기능 정도를 저해하고 삶의 질을 악화시키는 것으로 알려져 있다[12,13].
소아마비 환자에서 나타나는 백조목 변형은 특히 강직성 소아마비 환자들에서 흔하게 나타나며, 두 가지 양상의 변형으로 나뉜다. 우선 내재근의 강직으로 나타나는 피노케이토-번넬 검사 양성 백조목 변형이 있다. 앞서 소개한 바와 같이 내재근 유리술을 통하여 수술적 치료를 고려할 수 있다[44,47].
이와는 반대로 중수지 관절의 신전과 함께 백조목 변형이 있는 경우도 있는데, 이때는 내재근 구축보다는 수지 신전건의 과도한 긴장(overpull)에 의한 경우이다. 강직성 마비 환자에서 손목의 굴곡 구축이 있는 상태로 수년에 걸쳐 손가락을 능동적으로 신전하려는 노력이 반복적으로 작용하면 수지 신전건에 과도한 긴장 현상을 초래하여 백조목 변형이 일어난다. 이 경우에는 피노케이토-번넬 검사는 음성이다. 과도한 긴장에 의한 변형은 중앙건 절제술로 수지 신전건의 장력을 줄이는 방향으로 변형을 교정할 수 있다[48].
측부대 이전술을 시행 받은 소아마비 환자에서도 수술적 치료의 결과가 떨어지는 보고가 있어 수술적 치료를 적용할 때 유의해야 한다. 한 문헌에서는 5년 재발률을 40%까지 보고하였으며, 내재근 강직이 해결되지 않은 상태에서 측부대 이전술만으로는 불량한 결과를 보일 수 있다고 고찰하였다[49].
백조목 변형은 치료하기 어려운 변형이며 다양한 원인과 다양한 치료법이 있는 만큼 결과도 다양하다. 기존에 보고된 대표적인 결과들을 Table 3에 원인과 술기에 따라 정리하였다. 대체로 수술 후 결과들은 양호한 경과를 보이나, 완전한 호전은 어렵고 경미한 변형의 잔존을 동반하며, 수술 후에도 변형이 지속되는 경우가 있어 주의를 요한다.
다양한 수술 방법을 막론하고 많은 연구들에서 수술 후 합병증으로 잔존하는 변형, 특히 원위지 관절 신전 지연이 가장 빈번하게 발생하는 것으로 나타났다. 다만 기능적 예후에는 큰 영향을 끼치지 않는 것으로 생각된다. 이를 예방하기 위해 수술 전에 환자에게 수술 후에도 변형이 잔존할 수 있다는 설명과 함께 원위지 관절을 포함하는 술식을 함께 시행할 것인지에 대한 고민이 필요하다.
치료받지 않은 백조목 변형의 자연 경과가 어떠한지에 관한 직접적인 연구 결과는 없지만, 류마티스 관절염 환자가 백조목 변형이 있는 경우 병의 진행이 빨라 5년에서 10년 내로 관절 파괴가 진행하는 것으로 보고한 최근 연구가 있다[45]. 외상성 또는 다른 원인에 의한 백조목 변형에서는 변형의 진행이 사람마다 다르고 오랜 기간에 걸쳐 서서히 진행하는 것으로 보인다. 특히 Nalebuff 단계 1, 2인 경증 환자의 경우 기능적 불편함이 크지 않다면 환자와 상의 후 경과를 관찰하며 정기적으로 검진하도록 할 수 있겠다.
Notes
Funding
This study was supported by National Health Insurance Service Ilsan Hospital (grant No. NHIMC2021CR021).
Acknowledgements
We would like to express deep gratitude to Dr. Jin Soo Kim of the Plastic Surgery Department at Gwangmyeong Sungae Hospital for providing the surgical photos.
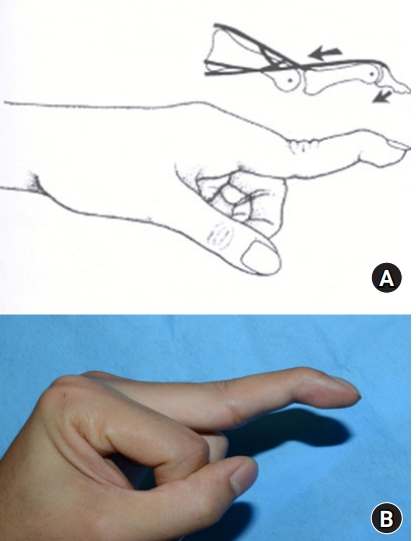
Fig. 3.
Positive Finochietto-Bunnell test in swan neck deformity of the finger with intrinsic muscle contracture. (A) When the proximal phalanx is in the extension position, it is impossible to flex the proximal interphalangeal joint. (B) However, flexion of the metacarpophalangeal joint allows proximal interphalangeal joint flexion.
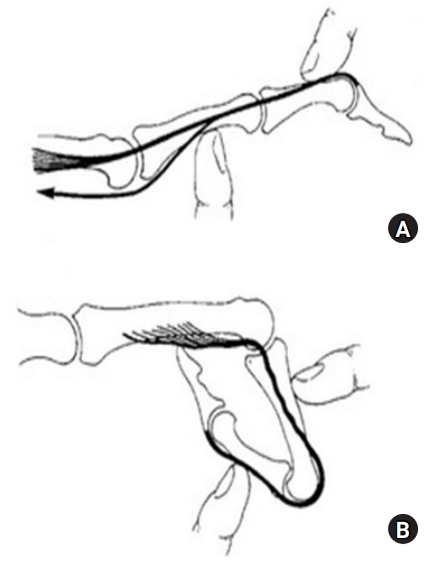
Fig. 4.
(A) Schematic drawing of modified tenodermodesis. (B) A 32-year-old man, injured 4 years ago, noted a painful dorsal bump and a 45° extension lag (arrow) in the distal interphalangeal joint (DIPJ). (C) After the Z-shaped skin incision, the subsequent extensor tendon was exposed over the DIPJ. (D) An elongated extensor tendon, including the joint capsule, was incised. (E) The dorsal osteophyte was trimmed with osteotomy. (F) After inserting a transaxial Kirschner wire (K-wire) in a fully extended DIPJ, the extensor tendon was repaired. (G, H) The redundant skin was incised, followed by separated skin sutures. The skin suture, tendon suture, and K-wire were sequentially removed at 2, 4, and 6 weeks. (I) Three months later, the deformity had improved.

Fig. 5.
Volar plate direct repair. (A, B) A 37-year-old man with a 70° hyperextension of the proximal interphalangeal joint (PIPJ) and 40° flexion contracture of the distal interphalangeal joint 3 months after an initial volar plate avulsion injury in the left small finger. (C) A Bruner-style lazy S-shaped incision was made over the PIPJ. (D) Between the flexor tendons, the injured volar plate was exposed. (E–G) After drilling, Mitek Micro QuickAnchor (DePuy Mitek Inc., Raynham, MA, USA) was inserted into the middle phalanx base, and the volar plate was sutured. (H) Photograph after the volar plate procedure was done. (I, J) At the final clinical follow-up, the finger showed an improved range of motion.

Fig. 6.
Flexor digitorum superficialis tenodesis; A2 pulley technique. (A) A Bruner-style lazy S-shaped incision at the volar side of the proximal interphalangeal joint and a transverse incision at the volar side of the metacarpophalangeal joint were made. (B, C) The radial slip of the flexor digitorum superficialis was identified through a metacarpophalangeal joint incision and transected from the metacarpophalangeal joint level. (D, E) The flexor digitorum superficialis slip was attached to the A2 pulley and knotted.
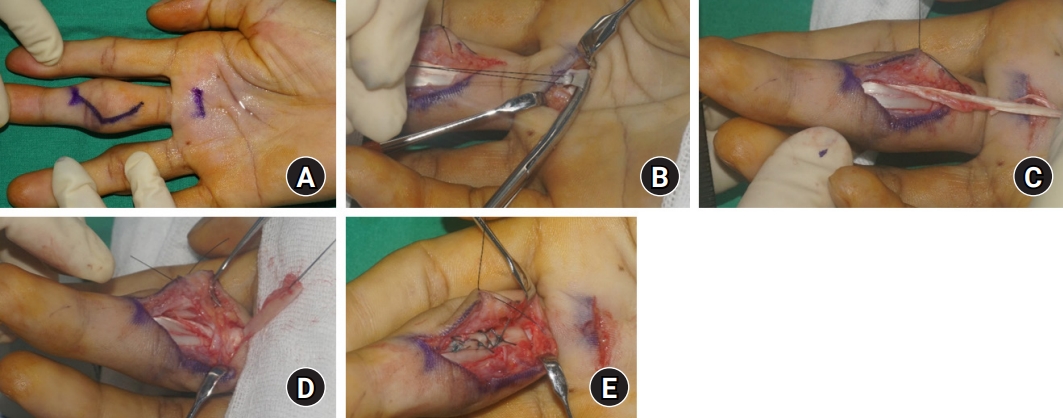
Fig. 7.
Flexor digitorum superficialis tenodesis; bone hole technique. (A, B) A 36-year-old man with 50° hyperextension of the proximal interphalangeal joint (PIPJ) and 30° flexion contracture of the distal interphalangeal joint 10 years after an initial chronic mallet finger injury to the right middle finger. (C) With a Bruner-style lazy S-shaped incision at the volar side of the PIPJ. (D) The radial side slip of flexor digitorum superficialis was transected from the proximal phalanx level, and the injured volar plate was exposed. (E, F) A 2-mm bone hole was made 1 cm proximal to the joint line through the proximal phalanx neck, and the harvested slip was knotted again through the hole. (G, H) An additional Mitek Micro QuickAnchor (DePuy Mitek Inc., Raynham, MA, USA) was inserted into the middle phalanx base, and the volar plate was repaired. (I) Photograph after flexor digitorum superficialis tenodesis and volar plate augmentation were done. (J, K) At the final clinical follow-up, the finger showed an improved range of motion.
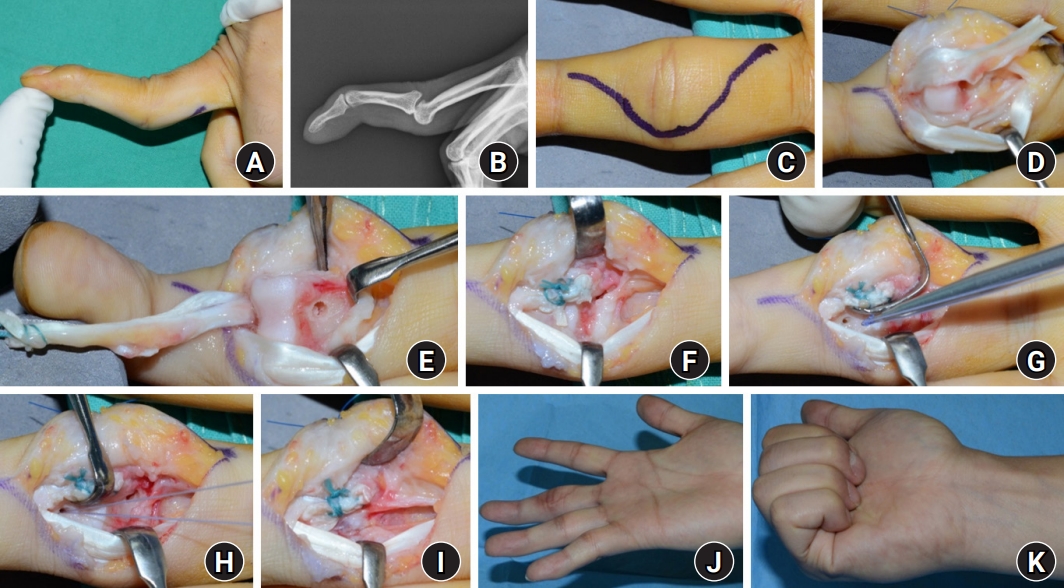
Fig. 8.
Oblique retinaculum ligament reconstruction. (A) A schematic drawing shows the concept of oblique retinaculum ligament reconstruction. (B, C) Swan neck deformity occurred after replantation surgery of the right index and middle finger amputation at the middle phalanx level. (D, E) The extensor digitorum longus tendons of the contralateral foot were harvested to reconstruct new ligaments. (F, G) The distal end was fixed using the pull-out technique. (H, I) A 2-mm bone hole was made in the shaft of the proximal phalanx. The proximal end of the tendon is inserted through the tunnel and fixed after graft tension adjustment. (J, K) At the final clinical follow-up, the finger showed an improved range of motion.
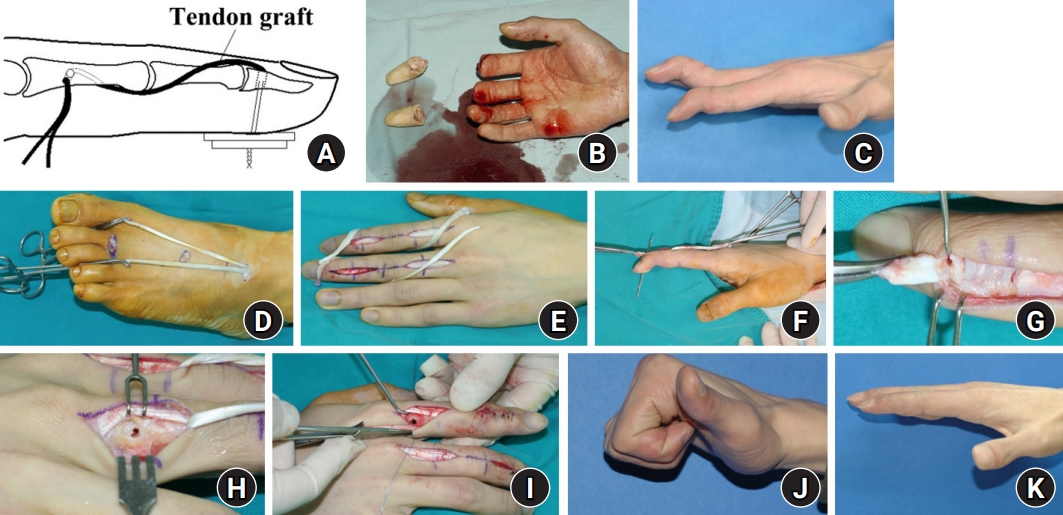
Table 1.
Classification of the etiologies of swan neck deformity by Zancolli [9]
Table 2.
Table 3.
Outcomes after surgical treatment of swan neck deformity
| Study | Year | Cause | Technique | Outcome |
|---|---|---|---|---|
| Iselin et al. [14] | 1977 | Mallet finger | Tenodermodesis | Satisfactory in 22 of 26 patients |
| 2 recurred deformities due to poor compliance | ||||
| 2 required a secondary arthrodesis | ||||
| Kon and Bloem [15] | 1982 | Mallet finger | Tenodermodesis | Satisfactory in 27 of 29 patients |
| 2 complications due to surgical site infection and inadequate distal tendon continuity | ||||
| Bowers and Hurst [22] | 1978 | Mallet finger | Central slip tenotomy | Among 5 patients, 4 excellent, 1 good |
| One good case had persistent DIPJ extension lag | ||||
| Lucas [23] | 1987 | Mallet finger | Central slip tenotomy | Satisfactory in 9 of 11 patients |
| 2 failed cases due to congenital flexion deformity and inadequate distal tendon continuity | ||||
| Grundberg and Reagan [25] | 1987 | Mallet finger | Central slip tenotomy | Satisfactory in all 20 patients |
| Average improvement of extension lag of DIPJ: 28° | ||||
| Houpt et al. [26] | 1993 | Mallet finger | Central slip tenotomy | Satisfactory in 34 of 35 patients |
| A failed case had residual extension lag: 30° | ||||
| Carlson et al. [48] | 2007 | Cerebral palsy | Central slip tenotomy | 33 fingers of 15 patients |
| Average improvement of extension lag of DIPJ: 32° | ||||
| Wollstein et al. [28] | 2006 | Chronic volar plate avulsion | Volar plate repair | Satisfactory in all 7 patients |
| No cases showed residual deformity | ||||
| Catalano et al. [34] | 2003 | Chronic volar plate avulsion | FDS tenodesis (FDP sheath) | Among 12 patients, 5 excellent, 5 good, 2 fair |
| 2 fair cases had postoperative PIPJ flexion contracture | ||||
| Brulard et al. [35] | 2012 | Rheumatoid arthritis | FDS tenodesis (A2 pulley) | Among 23 patients, 19 excellent and good, 4 fair |
| 4 fair cases had postoperative PIPJ flexion contracture | ||||
| Average improvement of range of motion of PIPJ: 61° | ||||
| Tonkin et al. [37] | 1992 | All | Lateral band mobilization | Satisfactory in all 30 patients |
| Average postoperative flexion contracture: 11° | ||||
| Gainor and Hummel [39] | 1985 | Rheumatoid arthritis | Lateral band mobilization | 57 fingers of 14 patients |
| 17 excellent, 21 good, 8 fair, 11 poor | ||||
| Poor cases due to severe rheumatoid arthritis flare | ||||
| Charruau et al. [38] | 2016 | All | Lateral band mobilization | 41 fingers of 14 patients |
| Satisfactory in all 14 patients | ||||
| Average active postoperative range of motion: 71° in PIPJ and 61° in DIPJ | ||||
| de Bruin et al. [49] | 2010 | Cerebral palsy | Lateral band mobilization | 62 fingers of 29 patients |
| Recurrence in 16% at 1-year follow-up, 40% at 5-year follow-up | ||||
| Oh et al. [41] | 2013 | Mallet finger | Spiral oblique retinacular ligament reconstruction | 27 fingers of 26 patients: 15 tendon grafts, 7 pull-outs, 5 anchors |
| No statistical difference in reconstructive technique | ||||
| 5 reoperations: 3 revisions due to graft rupture, 2 tenolysis | ||||
| Kanaya et al. [42] | 2013 | Mallet finger | Spiral oblique retinacular ligament reconstruction | Satisfactory in 6 of 7 patients |
| 1 buttonhole deformity due to inadequate graft tension | ||||
| Kleinman and Petersen [43] | 1984 | Mallet finger | Spiral oblique retinacular ligament reconstruction | Satisfactory in 10 of 12 patients |
| 2 reoperations: 1 graft lengthening, 1 tenolysis | ||||
| Matsuo et al. [47] | 2001 | Cerebral palsy | Intrinsic release | Satisfactory in all 32 patients |
| Improvement of daily living hand activities |
References
1. Kuczynski K. The proximal interphalangeal joint: anatomy and causes of stiffness in the fingers. J Bone Joint Surg Br. 1968;50:656-63.

2. Elzinga K, Chung KC. Managing swan neck and boutonniere deformities. Clin Plast Surg. 2019;46:329-37.


3. Fox PM, Chang J. Treating the proximal interphalangeal joint in swan neck and boutonniere deformities. Hand Clin. 2018;34:167-76.


4. Howell JW, Peck F. Rehabilitation of flexor and extensor tendon injuries in the hand: current updates. Injury. 2013;44:397-402.


5. McKeon KE, Lee DH. Posttraumatic boutonnière and swan neck deformities. J Am Acad Orthop Surg. 2015;23:623-32.


6. Adkinson JM, Johnson SP, Chung KC. The clinical implications of the oblique retinacular ligament. J Hand Surg Am. 2014;39:535-41.



7. Shrewsbury MM, Johnson RK. A systematic study of the oblique retinacular ligament of the human finger: its structure and function. J Hand Surg Am. 1977;2:194-9.


9. Zancolli E. Structural and dynamic bases of hand surgery. 2nd ed. Philadelphia: Lippincott; 1979. p. 64-79.
12. van der Giesen FJ, Nelissen RG, van Lankveld WJ, et al. Swan neck deformities in rheumatoid arthritis: a qualitative study on the patients’ perspectives on hand function problems and finger splints. Musculoskeletal Care. 2010;8:179-88.



13. Porter BJ, Brittain A. Splinting and hand exercise for three common hand deformities in rheumatoid arthritis: a clinical perspective. Curr Opin Rheumatol. 2012;24:215-21.


14. Iselin F, Levame J, Godoy J. A simplified technique for treating mallet fingers: tenodermodesis. J Hand Surg Am. 1977;2:118-21.


16. Georgescu AV, Capota IM, Matei IR. A new surgical treatment for mallet finger deformity: deepithelialised pedicled skin flap technique. Injury. 2013;44:351-5.


17. Murray PM. Treatment of the osteoarthritic hand and thumb. In: Wolfe S, Pederson W, Kozin SH, Cohen M, editors. Green’s operative hand surgery. 8th ed. Philadelphia: Elsevier; 2021. p. 345-372.
18. Han SH, Cha YS, Song WT. Arthrodesis of distal interphalangeal joints in the hand with interosseous wiring and intramedullary K-wire fixation. Clin Orthop Surg. 2014;6:401-4.



19. Lee JK, Lee S, Choi S, et al. Distal interphalangeal joint arthrodesis using only kirschner wires in small distal phalanges. Handchir Mikrochir Plast Chir. 2021;53:462-6.


20. Kiziridis G, Giddins GE. Volar tenodesis for the treatment of swan-neck deformity; a systematic review. J Hand Surg Asian Pac Vol. 2017;22:267-74.


21. Hiwatari R, Kuniyoshi K, Aoki M, Hashimoto K, Suzuki T, Takahashi K. Fractional Fowler tenotomy for chronic mallet finger: a cadaveric biomechanical study. J Hand Surg Am. 2012;37:2263-8.


22. Bowers WH, Hurst LC. Chronic mallet finger: the use of Fowler’s central slip release. J Hand Surg Am. 1978;3:373-6.


23. Lucas GL. Fowler central slip tenotomy for old mallet deformity. Plast Reconstr Surg. 1987;80:92-4.


24. Rozmaryn LM. Central slip tenotomy with distal repair in the treatment of severe chronic mallet fingers. J Hand Surg Am. 2014;39:773-8.


25. Grundberg AB, Reagan DS. Central slip tenotomy for chronic mallet finger deformity. J Hand Surg Am. 1987;12:545-7.


26. Houpt P, Dijkstra R, Storm van Leeuwen JB. Fowler’s tenotomy for mallet deformity. J Hand Surg Br. 1993;18:499-500.



27. Eaton RG, Malerich MM. Volar plate arthroplasty of the proximal interphalangeal joint: a review of ten years’ experience. J Hand Surg Am. 1980;5:260-8.


28. Wollstein R, Watson HK, Carlson L. A technique for the repair of chronic volar plate avulsion of the proximal interphalangeal joint: a review of 54 cases. Plast Reconstr Surg. 2006;117:1239-47.


29. Nalebuff EA, Millender LH. Surgical treatment of the swan-neck deformity in rheumatoid arthritis. Orthop Clin North Am. 1975;6:733-52.


30. Curtis R. Sublimis tenodesis. In: Edmonson A, Crenshaw A, editors. Campbell’s operative orthopaedics. 6th ed. St. Louis: C.V. Mosby; 1980. p. 319.
31. Karthaus RP, van der Werf GJ. Operative correction of posttraumatic and congenital swanneck deformity-a new technique. J Hand Surg Br. 1986;11:239-42.



32. Wei DH, Terrono AL. Superficialis sling (flexor digitorum superficialis tenodesis) for swan neck reconstruction. J Hand Surg Am. 2015;40:2068-74.


33. Caviglia D, Ciolli G, Fulchignoni C, Rocchi L. Chronic post-traumatic volar plate avulsions of the finger proximal interphalangeal joint: a literature review of different surgical techniques. Orthop Rev (Pavia). 2021;13:9058.




34. Catalano LW 3rd, Skarparis AC, Glickel SZ, et al. Treatment of chronic, traumatic hyperextension deformities of the proximal interphalangeal joint with flexor digitorum superficialis tenodesis. J Hand Surg Am. 2003;28:448-52.


35. Brulard C, Sauvage A, Mares O, Wavreille G, Fontaine C. Treatment of rheumatoid swan neck deformity by tenodesis of proximal interphalangeal joint with a half flexor digitorum superficialis tendon: about 23 fingers at 61 months follow-up. Chir Main. 2012;31:118-27.

36. Littler JW. Restoration of the oblique retinacular ligament for correcting hyperextension deformity of the proximal interphalangeal joint. In: Tubiana R, editor. La main rhumatismale. Paris: Expansion Scientifique Francaise; 1966. p. 159-67.
37. Tonkin MA, Hughes J, Smith KL. Lateral band translocation for swan-neck deformity. J Hand Surg Am. 1992;17:260-7.


38. Charruau B, Laulan J, Saint-Cast Y. Lateral band translocation for swan-neck deformity: outcomes of 41 digits after a mean follow-up of eight years. Orthop Traumatol Surg Res. 2016;102(4 Suppl):S221-4.

39. Gainor BJ, Hummel GL. Correction of rheumatoid swan-neck deformity by lateral band mobilization. J Hand Surg Am. 1985;10:370-6.


40. Thompson JS, Littler JW, Upton J. The spiral oblique retinacular ligament (SORL). J Hand Surg Am. 1978;3:482-7.


41. Oh JY, Kim JS, Lee DC, et al. Comparative study of spiral oblique retinacular ligament reconstruction techniques using either a lateral band or a tendon graft. Arch Plast Surg. 2013;40:773-8.



42. Kanaya K, Wada T, Yamashita T. The Thompson procedure for chronic mallet finger deformity. J Hand Surg Am. 2013;38:1295-300.


43. Kleinman WB, Petersen DP. Oblique retinacular ligament reconstruction for chronic mallet finger deformity. J Hand Surg Am. 1984;9:399-404.


44. Carlson EJ, Carlson MG. Treatment of swan neck deformity in cerebral palsy. J Hand Surg Am. 2014;39:768-72.


45. Toyama S, Tokunaga D, Tsuchida S, et al. Comprehensive assessment of alterations in hand deformities over 11 years in patients with rheumatoid arthritis using cluster analysis and analysis of covariance. Arthritis Res Ther. 2021;23:66.




46. Borisch N, Haubmann P. Littler tenodesis for correction of swan neck deformity in rheumatoid arthritis. Oper Orthop Traumatol. 2011;23:232-40.



47. Matsuo T, Matsuo A, Hajime T, Fukumoto S, Chen W, Iwamoto Y. Release of flexors and intrinsic muscles for finger spasticity in cerebral palsy. Clin Orthop Relat Res. 2001;(384):162-8.