Proximal bifurcation of the superficial palmar branch of the radial artery and anomalous superficial course of the distal radial artery: a case report
Article information
Abstract
Variations of the radial artery are rare, but clinically significant for surgeons when raising a radial forearm free flap. A 68-year-old man presented with an anomaly of the radial artery, which had a proximal bifurcation of the superficial palmar branch and an anomalous superficial course of the distal radial artery, mimicking duplication of the radial artery. A bifurcation of the main vessel was detected approximately 7 cm proximal to the wrist crease. Anastomosis was performed by using the superficial palmar branch of the radial artery. After anastomosis, the anomalously bifurcated deep palmar branch of the radial artery was transected 1 cm distal to the bifurcation. Although variations, such as unusual bifurcations of the radial artery, are extremely rare, surgeons should be aware of possible variations to ensure safe flap harvesting.
Introduction
The radial forearm free flap is an essential method for reconstruction of the head and neck. Although the course of the radial artery, which lies between the flexor carpi radialis (FCR) and brachioradialis (BR) muscles, is thought to be fairly constant, seldom encountered anomalies that are found during the elevation of the flap have been reported [1-3]. Proximal bifurcation is one such rare variant of the distal radial artery, with an incidence of 0.52%–1% [4].
This report describes a proximal bifurcation of the superficial palmar branch and anomalous superficial course of the distal radial artery.
Case report
This case report was approved by the Institutional Review Board of the Korea University Ansan Hospital (No. 2020AS0050). Written informed consent was obtained for publication of this report and accompanying images.
A 68-year-old male patient with the chief complaint of a tongue mass was diagnosed with T2N2bM0 squamous cell carcinoma. He was scheduled for hemiglossectomy, followed by immediate tongue reconstruction using a left-sided radial forearm free flap. On preoperative examination, the radial and ulnar artery pulses were both palpable at their respective normal sites, and the Allen test confirmed adequate blood flow in both the radial and ulnar arteries. The course of the radial artery was traced more proximally using handheld Doppler ultrasound, following the continuity of the signals. Sensory and motor functions of the left hand were normal.
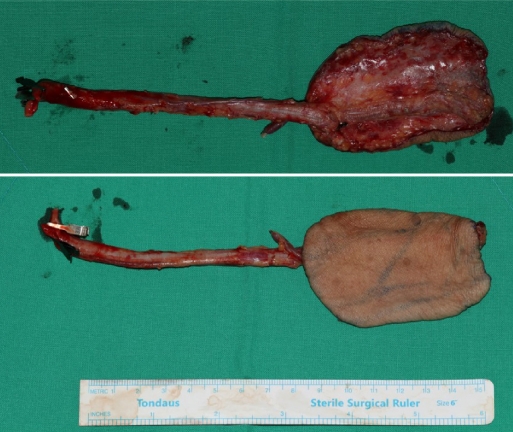
After hemiglossectomy, an 8×6 cm sized radial forearm flap was designed on the left palmar-sided distal forearm, and the tourniquet was inflated to 250 mmHg after exsanguination by elevation. Starting elevation of the flap in the suprafascial plane at the ulnar border, elevation proceeded superficially to the tendinous portion of the palmaris longus, dividing the intermuscular septa, until reaching the tendinous portion of the FCR. At this point, the distal end of the radial artery and the accompanying veins were identified just at the interval between the muscular portion of the FCR and BR. The pedicle was ligated and divided to allow the flap to be raised from the distal to the proximal direction.
After the radial incision, we identified the cephalic vein and dissected it subcutaneously and proximally following this vein to identify the superficial branches of the radial nerve. Another pedicle consisting of one artery and two accompanying veins was observed just beneath the superficial branch of the radial nerve in the subcutaneous layer. Superficial to the BR muscle, it coursed radially and crossed the superficial branch of the radial nerve, extending in the distal and dorsal directions in the wrist (Fig. 1). The forearm was then incised and dissected proximally following the anomalous branch to confirm merging with the main radial artery. We confirmed that the main trunk of the vessel was bifurcated into two branches, approximately 7 cm proximal to the wrist crease (Fig. 2).
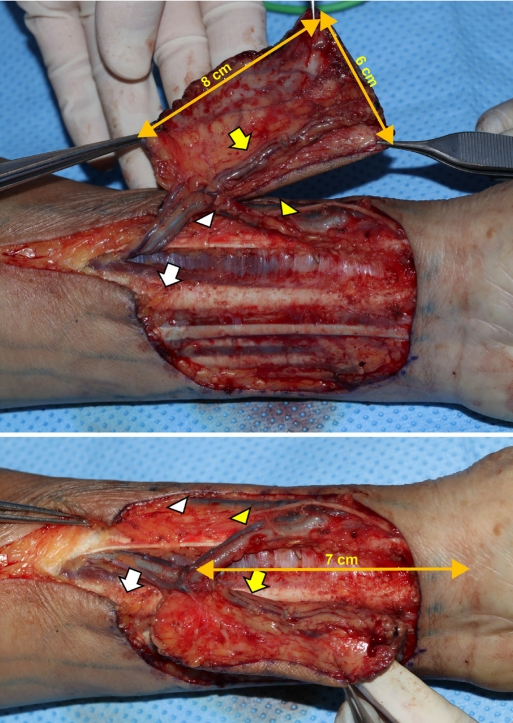
Dissected radial artery and vein between the flexor carpi radialis muscle (white arrows) and the brachioradialis muscle (white arrowheads). Proximal bifurcation of the radial artery into the superficial palmar branch (yellow arrows) and the dorsal carpal branch (yellow arrowheads).
The tourniquet was then released and the original pedicle, which normally lies between the tendinous portion of the FCR and BR, was confirmed to perfuse the skin territory when the anomalous branch was obstructed with a vessel clamp. We performed the Allen test intraoperatively and observed sufficient blood flow from the ulnar circulation. The anomalous branch was then divided at a point 1 cm distal to bifurcation. Microvascular anastomosis in the end-to-end method was performed with the superior thyroidal artery and internal jugular vein, and arterial and venous flows were sufficient. No complications were associated with postoperative flap circulation.
Discussion
At the wrist, the usual radial artery branches off the superficial palmar branch and continues dorsally deep to the tendons of the first and third extensor compartments. It provides a deep palmar branch for the formation of the deep palmar arch in the radial foveola (anatomical snuffbox), and joins the deep palmar arch. As the radial arterial system is much more reliable than other arterial systems, preoperative evaluation with an imaging device is considered unnecessary if the results of Allen test are normal.
Several variations of the radial artery have been reported in the literature [3,5,6], particularly in the context of harvesting radial forearm flaps. In previous studies, various anomalies such as radial artery branching not from brachial artery but from common interosseous artery, and aberrant collateral artery have been reported. In our case, abnormal branching of the main vessel was observed in the distal third of the forearm (Fig. 3). A branch that coursed in the usual anatomic position of the radial artery appeared to be the proximally bifurcated superficial palmar branch, whereas the anomalous branch that coursed superficial to the anatomical snuffbox was considered to be the distal radial artery. The anomalous artery would have been open when the superficial palmar branch was occluded during the Allen test, causing the collateral circulation of the ulnar artery to be poorly assessed. Preoperative vascular imaging was performed using Doppler sonography rather than ultrasound, which makes it difficult to detect the anomalous course of the distal radial artery.
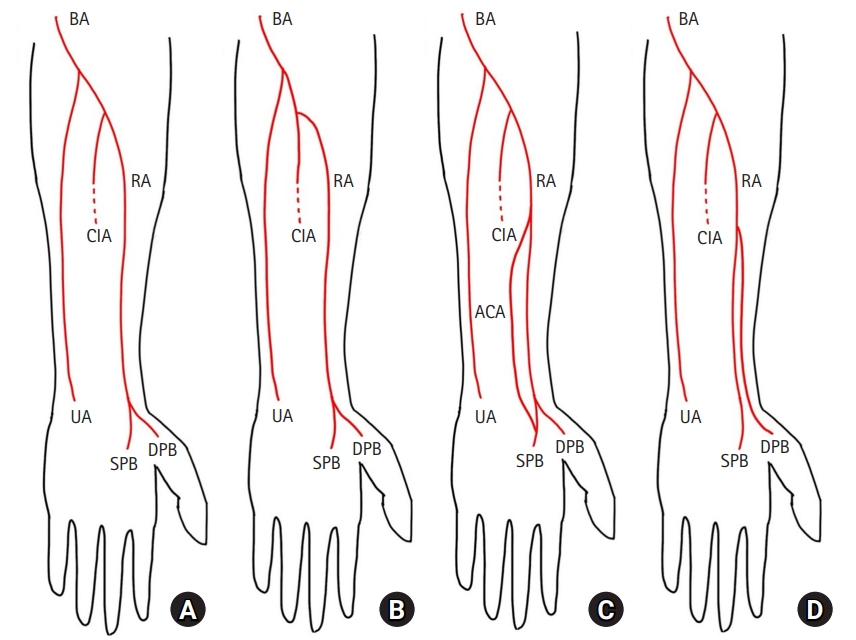
Schematic courses of previously reported anomalies. (A) Normal course of the radial artery (RA). (B) RA branching not from the brachial artery (BA), but from the common interosseous artery (CIA). (C) Aberrant collateral RA. (D) Proximal bifurcation of the superficial palmar branch of the RA (SPB). UA, ulnar artery; DPB, deep palmar branch of the RA; ACA, aberrant collateral radial artery.
An anomalous superficial course of the radial artery, similar to this case, has been reported as a superficial radial artery, but such cases are quite scarce [1,2]. There are some reports of variations in the radial artery. Superficial courses, such as proximal bifurcation [6,7] and distal radial artery, have been reported [5,6] but are not actively discussed as notable variations [2]. During embryologic development, the arterial variations affecting these kinds of distal courses of the radial artery are expected to be established before embryonic developmental stage 21 (crown-lump length, 22–24 mm) [8].
The Allen test was positive because the anomalous branch maintained circulation even when the radial side was occluded. Usually, imaging tests for vessels are not necessarily performed [9], and these anatomical variations may not be detected before surgery, which could lead to severe surgical complications [10]. Therefore, surgeons should elevate the flap carefully, considering the possibility of vascular variations, and we recommend retaining branches until the circulation of the flap is confirmed. The vessels should be carefully evaluated to determine whether they can be used as the main vascular pedicle.
In this case, a radial forearm free flap was chosen for reconstruction of the tongue defect after tumor resection. It appeared to be a proximally bifurcated deep palmar branch of the radial artery. The superficial palmar branch of the radial artery was used as the main vascular pedicle for the flap.
Despite its rare incidence (0.52%–1%), anomalies of the radial artery exist. Reconstructive surgeons should be aware of these anomalies, and preoperative ultrasound evaluation is suggested to detect an anomalous course of the distal radial artery for safe flap harvesting.
Notes
The authors have nothing to disclose.
Funding
None.