Clinical analysis of the communicating artery between the dorsal and plantar aspects of the foot
Article information
Abstract
Purpose
One of the treatment methods for critical limb ischemia is percutaneous transluminal angioplasty (PTA). In severe cases, however, multiple vessels are blocked, including the main vessels of the lower extremities. This study aimed to determine whether wound healing and symptom relief occurred depending on whether the communicating artery was patent after PTA.
Methods
In total, 120 patients (120 lower extremities) who underwent PTA from January 2016 to February 2018 were followed up for 6 months.
Results
Out of 87 patients who had wounds, 34 had a patent communicating artery and 53 had a non-patent communicating artery. Out of 34 patients who had wounds but a patent communicating artery, 29 completely healed within 6 months. Among the 53 patients who had wounds and a non-patent communicating artery, 16 totally healed within 6 months, and 37 did not heal within 6 months. In the indirect revascularization group, 18 of 21 patients with complete wound healing within 6 months in the indirect revascularization group had a patent communicating artery.
Conclusion
If only indirect revascularization is possible, it is important to ensure the patency of the communicating vessels that link the pedal and plantar arterial systems.
Introduction
Peripheral arterial occlusive disease (PAOD) is characterized by decreased perfusion of blocked vessels due to stenosis or occlusion. The most common cause of PAOD is atherosclerosis. More than 200 million people worldwide have PAOD, which is defined as an ankle-brachial index (ABI) less than 0.9, and this number is growing [1]. Only one-quarter of people with PAOD show symptoms [2].
Critical limb ischemia (CLI) is the most severe clinical finding of peripheral vascular disease. CLI can cause skin ulcers, necrosis, and amputation of tissue as a result of gradual ischemia of the lower extremity blood vessels, which can lead to serious ischemic pain even when stabilized. It is estimated that 15% to 30% of the patients with PAOD progress from intermittent claudication to CLI, which affects 1% of adults after the age of 50 years. An estimated 15 million to 20 million people in the United States and Europe are suffering from CLI. In addition, approximately 150,000 patients with CLI undergo limb amputation in the same regions each year. A year after CLI onset, about 25% of the patients die, and 25% of them are amputated [3].
There are some risk factors for PAOD and CLI such as age, increased body mass index (BMI), diabetes mellitus, hypertension, tobacco use, hyperlipidemia, cardiac status, carotid status, renal disease, pulmonary status, and amputation history [4]. In limb- or life-threatening cases, a radical approach from both internal medicine and surgical departments is required [2]. Ideally, care should be carried out in cooperation with various surgical, interventional, and medical experts. To overcome PAOD and CLI, revascularization with sufficient perfusion is essential.
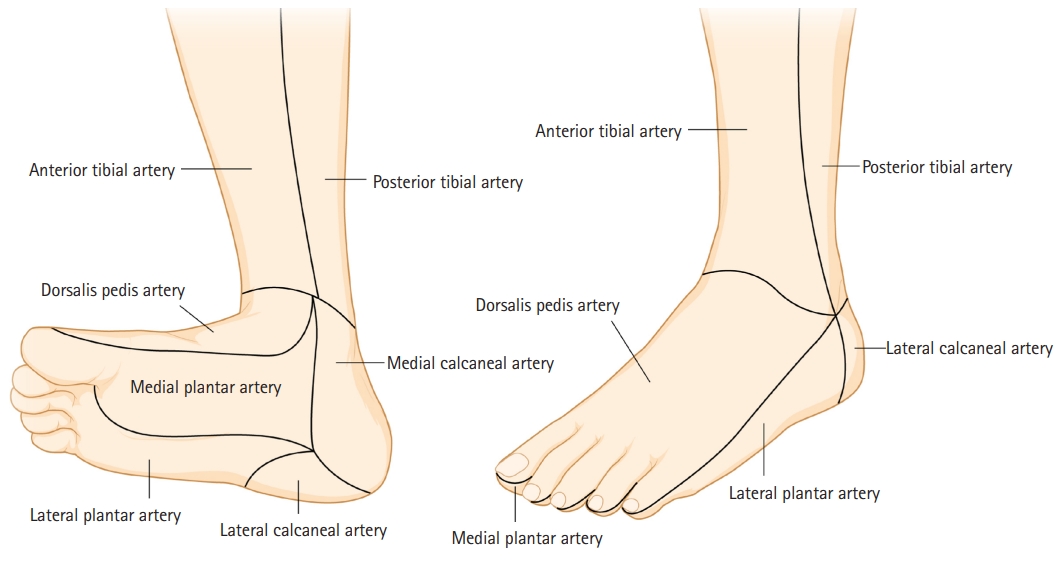
One of the treatment options for PAOD is percutaneous transluminal angioplasty (PTA). Recently, the selection of the artery for revascularization has been at the center of debate. A new approach, the concept of angiosome, which is the skin territory vascularized by a source artery, has been introduced (Fig. 1). Two meta-analyses found angiosome-targeted (direct) revascularization to be better than non-targeted (indirect) revascularization [5,6]. Although there is still a debate on which approach leads to a better result, it is generally known that following the concept of angiosome is beneficial. In severe patients, however, multiple vessels are blocked, including the main vessels of the lower extremities, and the choice of treatment must take into consideration the patient’s condition.
Direct revascularization is performed according to the concept of angiosome, but in some cases, if PTA is difficult to be performed due to severe blockage of blood vessels, indirect revascularization is performed by using collateral vessels and perforating arteries. For example, blood flow may return from the plantar artery to the dorsal artery, so by assuring plantar arterial system patency, it can be possible to achieve partial arterial blood flow patency in the pedal arterial system. The vessels used in this procedure are the distal communicating and deep plantar artery or deep perforating artery, termed communicating artery, between the dorsalis pedis and the medial and lateral plantar arteries (Fig. 2).

Diagram of a communicating artery, consisting of a distal communicating artery and a deep plantar artery.
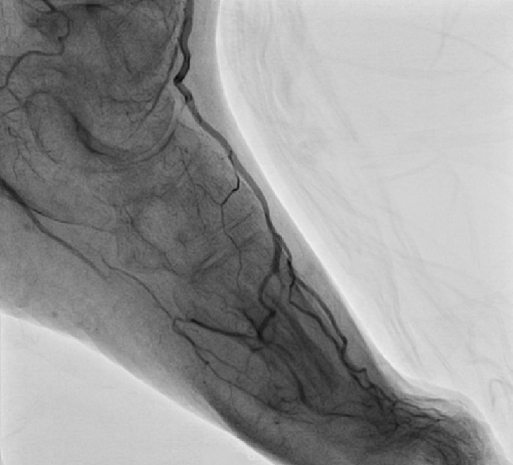
For example, communicating artery (asterisk in Fig. 3) is shown in the foot of a patient with CLI patient (anteroposterior angiographic projection). The dorsalis pedis artery is connected via the communicating artery in the first metatarsal space with the plantar artery (Fig. 3). Preoperatively, plantar artery is not shown (Fig. 4), but postoperatively retrograde plantar flow is shown (Fig. 5). Finally, plantar arterial flow became clearer than before the intervention (Fig. 6).
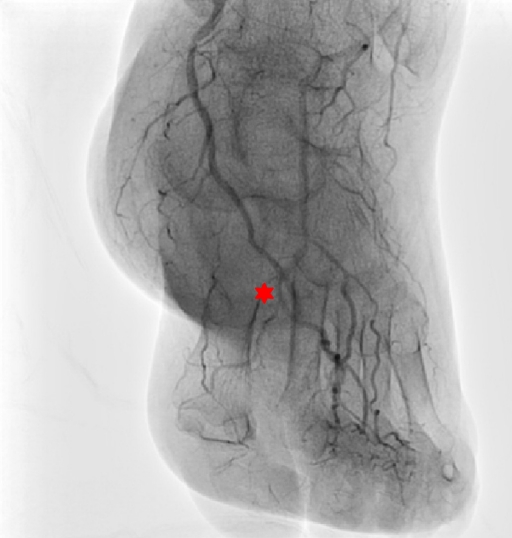
The communicating artery (*) is shown in the foot of a patient with critical limb ischemia (anteroposterior angiographic projection). The dorsalis pedis artery is connected via the communicating artery in the first metatarsal space with the plantar artery.

Postoperative latero-oblique angiographic projection. Retrograde plantar flow is shown through the communicating artery from the dorsalis pedis artery.
After 2 seconds, the plantar arterial flow became clearer due to retrograde flow via the communicating artery.
The aim of this study was to determine whether wound healing (Rutherford 5, 6) and symptom relief (Rutherford 1–4) occur depending on whether the communicating artery is patent after PTA, and to investigate the clinical significance of the communicating artery.
Methods
Ethics statement: The study protocol was approved by the Institutional Review Board of Soonchunhyang University College of Medicine (No. 2022-05-022). The requirement for informed consent was waived because of the retrospective nature of the study. All medical records in the study involving human participants were reviewed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
From January 2016 to February 2018, a retrospective study was done at Soonchunhyang University Hospital Cheonan. Inclusion criteria were undergoing PTA of a lower extremity at our clinic. A total of 227 patients who had lower extremity wounds or symptoms were included in the study. All procedures and photographs were taken after sufficient explanation and patient consent.
Exclusion criteria were a history of major amputation (except toe amputation), a history of traumatic vessel injury or bypass surgery, a follow-up period shorter than 6 months, and missing medical record data, such as those of past history. Patients with wounds or symptoms on both lower extremities and who underwent PTA or staged-PTA for both lower extremities were also excluded. After applying the exclusion criteria, 120 patients (120 lower extremities) were eligible for the study. All patients’ symptoms and wounds were followed up for at least 6 months, and the patency of communicating artery was recorded before and after PTA.
Based on whether the communicating artery was patent after PTA, it was determined whether the wound fully healed within 6 months; symptom relief was also recorded. In order to objectify and record the recovery process of symptoms or wounds, the Rutherford grade system, currently the most widely used of the ischemic diseases of the lower extremities, was used. But Rutherford grade system classifies a wound into only two categories. So the University of Texas classification system and Wagner classification were used to refine the wound to compensate for the lack of the Rutherford system.
Symptom relief was determined by a decrease in the Rutherford grade classification. Wound healing was assessed depending on whether full healing had occurred within 6 months without progression to chronic hard-to-heal wound. In most cases, wound healing occurs within 12 weeks. Only patients with no wound signs after 6 months were considered to achieve full healing.
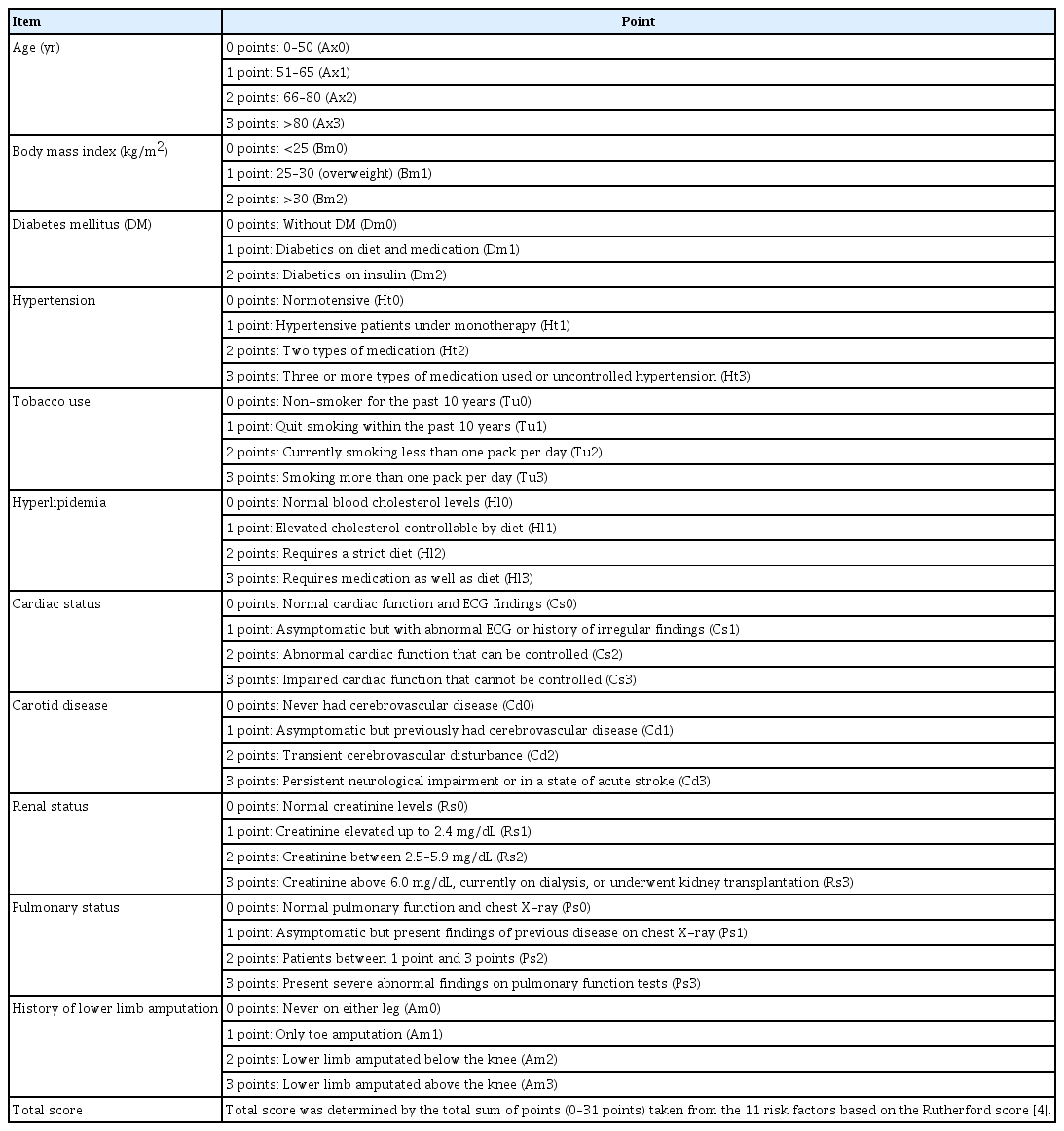
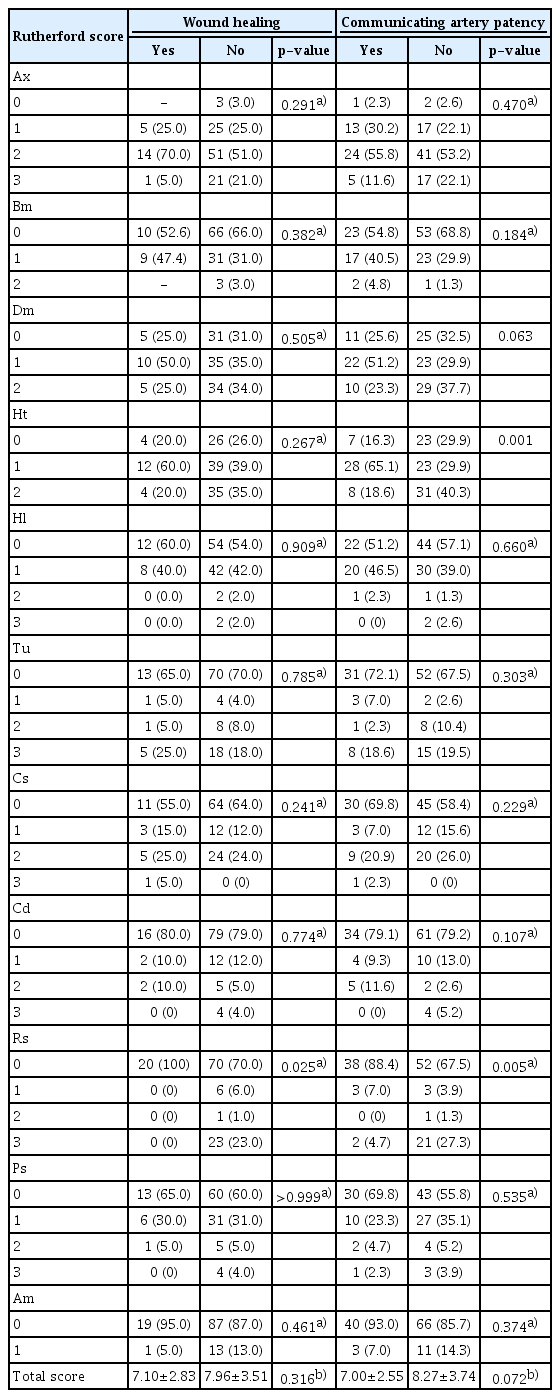
Data concerning 11 risk factors including age, BMI, diabetes mellitus, hypertension, tobacco use, hyperlipidemia, cardiac status, carotid status, renal disease, pulmonary status, and history of lower limb amputation were collected. Each risk factor was classified according to the Rutherford scoring system to evaluate the effect of each risk factor on communicating artery occlusion (Table 1) [4].
In accordance with the concept of angiosome, the wound healing ratio was determined by comparing direct and indirect revascularization. The effect of communicating artery patency on wound healing was evaluated in the indirect revascularization group.
Diagnostic angiography was performed from two different angles. In order to accurately identify the location and measure the length of the lesion, using a ruler was recommended. Calcification grade and the number of distal runoff vessels were evaluated. The classification of calcified lesion was classified into none, mild, moderate, and severe calcification. Interventional physicians used balloon angioplasty or stent implant. The duration of balloon dilation should last at least 120 seconds. Afterward, if there was residual stenosis of >30%, flow-limiting dissection, or residual pressure gradient of >10 mmHg, provisional stenting was done. Stent deployment should have been performed in an area where there is no significant stenosis (less than 30% stenosis), and up to 10 mm proximally and distally from the target lesion was permitted. Criteria for successful stent implantation are residual stenosis of <30% and residual pressure gradient of <10 mmHg. Measurements of reference vessel diameter, minimal luminal diameter, percentage of stenosis diameter, and acute gain were done. We used Allura clarity (Philips, Andover, MA, USA), and the nonionic isosmolar contrast medium iodixanol (containing 270 mg/mL of iodine) with a power injector. Occasionally, additional dye is needed for optimal vascular enhancement due to poor runoff in critically diseased vessels. A frame rate of one frame per second is usually employed in filming. Prolonged filming is often necessary to record delayed enhancement of pedal vessels by contrast material from collateral or retrograde circulation. After PTA, communicating artery patency was determined.
1. Statistical processing
The statistical analysis was performed using IBM SPSS Statistics for Windows ver. 25 (IBM Corp., Armonk, NY, USA). Continuous data were expressed as mean±standard deviation or median (interquartile range) as appropriate. Categorical data were expressed by frequency (proportion, %). A chi-square test or Fisher exact test was used for categorical data as appropriate. Continuous variables were compared between the two groups using Student t-test or the Mann-Whitney U-test as appropriate. The wound healing ratio and symptom relief were compared between the communicating artery patency and no-patency groups using Pearson chi-square or Fisher exact test. Additionally, the wound healing and communicating artery patency ratios were compared between the direct and indirect revascularization groups using Pearson chi-square test or Fisher exact test. A two-sided p-value less than 0.05 was considered to indicate statistical significance.
Results
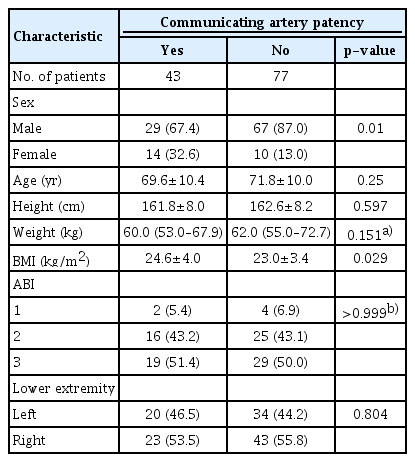
A total of 120 patients (120 lower extremities) were studied. Ninety-six patients were male. Communicating artery patency was observed in 43 patients and non-patency was observed in 77 patients. The median patient age in the patent and non-patent communicating artery groups was 69.6 and 71.8, respectively. Regarding the ABI, two patients had ABI of >1.3, 16 patients had ABI of ≤1.3 and ≥0.9, and 19 patients had ABI of <0.9 in the communicating artery patency group. In the non-patent communicating artery group, four patients had ABI of >1.3, 25 patients had ABI of ≤1.3 and ≥0.9, and 29 patients had ABI of <0.9. There were no significant differences between the compositions of the two groups (Table 2).
Out of the 120 patients, the communicating artery was present before PTA in 20 patients. Eighty-seven patients had wounds and 33 were only symptomatic not wounds. Among the 87 patients with wounds, 34 and 53 had a patent and non-patent communicating artery, respectively.
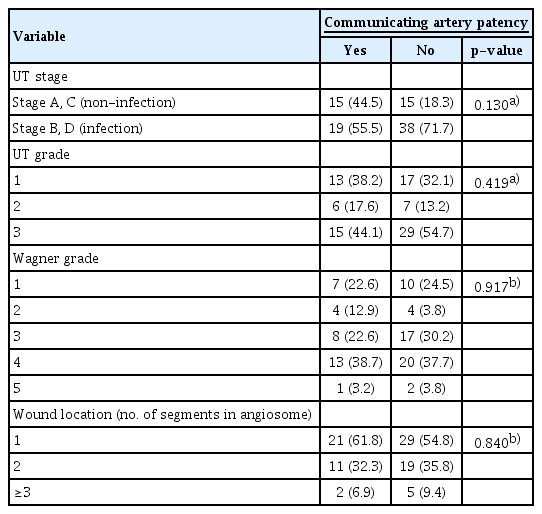
For the 87 patients with wounds, the location of wound was divided into six zones according to the angiosome concept (Fig. 1). Of the 34 patients with the patent communicating artery, 21 patients had wounds in one area, 11 patients had wounds in two areas, and two patients had wounds in three or more areas. Of the 53 patients with the non-patent communicating artery, 29 had wounds in one area, 19 had wounds in two areas, and five had wounds in three or more areas. The number of zones containing wounds did not show statistically significant differences, according to the status of the communicating artery (Table 3). There were no statistical differences in the analysis of the infection ratio, with 19 out of 34 patent group and 38 out of 53 non-patent group (Table 3).
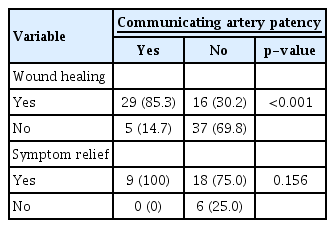
Of the 34 patients who had wounds and a patent communicating artery, 29 were fully healed within 6 months, and five were not healed within 6 months. Of the 53 patients who had wounds and a non-patent communicating artery, 16 were fully healed within 6 months, and 37 were not healed within 6 months. After PTA, it was statistically significant that the full wound healing rate was higher in the patent than in the non-patent communicating artery group (p<0.001) (Table 4).
Out of the 33 patients who had symptoms but not wounds, communicating artery patency and non-patency were observed in nine and 24 patients, respectively. All nine patients with a patent communicating artery achieved full symptom relief. Eighteen of the 24 patients with a non-patent communicating artery were fully relieved of their symptoms. The other six patients did not achieve symptom relief after PTA. However, there was not a significant difference (p=0.156) (Table 4).
The relationship among history, wound healing, and the patency of the communicating artery based on the Rutherford scoring system is shown [4]. In general, the higher the history score, the more likely it was for wounds not to be healed and for the communicating artery to be non-patent after PTA. Renal status was also found to significantly influence wound healing. The factors influencing communicating artery patency were renal status and hypertension (p<0.05). Regarding the total score, the median score of patients with and without full healing of the wound was 7.10±2.83 and 7.96±3.51, respectively. As for communicating artery patency, the median score of patent and non-patent groups was 7.00±2.55 and 8.27±3.74, respectively. The non-healed and non-patent groups had a slightly higher score, but this difference did not reach a statistical significance value (Table 5).
All of the 87 patients with wounds had dominant vessel occlusion grade ≥2 (more than 50% of vessel wall), according to the angiosome concept. Dominant vessel revascularization group was termed direct revascularization group and the non-dominant vessel revascularization group was termed indirect revascularization group. The direct and indirect revascularization groups had 49 and 38 patients, respectively. Twenty-four patients of the direct revascularization group had full wound healing within 6 months, and the remaining 25 patients’ wounds had not healed within 6 months. In the indirect revascularization group, 21 patients had full wound healing within 6 months, and the remaining 17 patients’ wounds had not healed within 6 months. There was no difference in the results between these two groups (Table 6).
Regarding communicating artery patency and wound healing, 18 of 21 patients with full wound healing within 6 months in the indirect revascularization group had a patent communicating artery patent group, while the remaining 3 had a non-patent communicating artery. In the indirect revascularization group, only two of 17 patients without full wound healing within 6 months had a patent communicating artery, while the remaining 15 patients had a non-patent communicating artery (Table 7).
Discussion
Despite the benefits of pharmacologic therapy, arterial revascularization remains the mainstay of CLI treatment because restoring adequate blood flow to the foot is crucial to provide pain relief, promote wound healing, and avoid amputation.
Attinger et al. [7] developed the angiosome concept introduced by Taylor and Palmer [8] for use in the clinical treatment of foot and ankle. Foot and ankle were divided into six territories, each supplied by a particular artery. A recent study shows that the restoration of vascular supply according to this concept leads to better clinical results [9].
The vascular anatomy of the foot consists of the anterior and posterior circulatory pathways that are connected through the pedal arches [10]. If direct revascularization with an antegrade approach is impossible, then a retrograde approach through the pedal-plantar anastomosis may be needed, which was termed communicating artery in this study [11,12]. The main pedal-plantar anastomosis is the pedal-plantar loop, which consists of the anastomosis of the dorsalis pedis artery in the first metatarsal space, the plantar arch, and the lateral plantar artery through the deep perforating artery [12]. The deep pedal arch, which links the medial plantar and medial tarsal arteries and the distal communicating artery at the level of the metatarsal head, can also form an anastomosis between the pedal and plantar arteries.
The importance of the anatomic anastomosis between the anterior and posterior circulation has been known for almost 25 years [13]. There is a general belief that the communicating artery plays an important role in foot and ankle revascularization; however, not many studies have been conducted. Although several studies have dealt with the relationship between the communicating artery and amputation or survival rates, there have been no studies dealing with the relationship between the communicating artery and wound healing, especially between interventional part and surgical part [14].
According to recent studies, in patients with ischemic wounds, direct revascularization is considered the best treatment [7,8]. However, direct revascularization is often difficult when several vessels are blocked at the same time, which often requires selective treatment. For example, in the case of the hallux, which is vascularized by the first metatarsal artery originating from the dorsalis pedis and medial and lateral plantar arteries, when it is not possible to revascularize these vessels at the same time, the dominant vessel should be identified and selected for revascularization. However, if the dominant vessel revascularization fails, there is no choice but to conduct indirect revascularization. In the case of indirect revascularization, the authors consider better results can be achieved if there is a patent communicating artery, the link between the pedal arterial system and the plantar arterial system.
In the 87 patients with wounds, the rate of full wound healing after 6 months was statistically significantly higher in the patent communicating artery group. In this group, most patients had full wound healing within 12 weeks, and the rest only needed minimal dressing. This suggests that communicating artery patency is a factor that can increase the wound healing rate. Once it is confirmed that the vessels linking the plantar and pedal arterial system are healthy, even if there is a problem on either side, these systems may complement each other, unlike in cases of non-patency, thus lowering the probability of a blood supply problem in the corresponding area.
The reason why the criteria for the wound healing was set at 6 months was that hard-to-heal wound, defined as a wound that did not heal for more than 6 months, had more bias as more various treatments were attempted from this time. In addition, our hospital mainly treats high-level patients, and if their conditions get improved, we induce them to follow lower-level hospitals or self-treatment. And in the cases of successful PTA, it is usually reevaluated after 6 months, so it was based on the criteria to reduce bias.
Our findings indicate that plastic surgeons can tell patients that wounds can be healed through proper wound dressing when the communicating artery is patent, and also suggest the implementation of multiple approaches such as managing life habits in consultation with other departments. Conversely, if the communicating artery is not patent, plastic surgeons should explain that the current vessel status is more likely to cause a relapse, and if other factors are not managed, the wound is more likely to worsen and consider amputation.
In our study, the relationship between history factors, wound healing, and communicating artery patency was found to be nonsignificant except for renal status and hypertension. This is thought to be due to the poor health status of patients who underwent PTA. Patients undergoing PTA at our hospital are predominantly elderly or in poor condition, so they do not constitute a good example of a single group to determine why blood vessels are obstructed.
Differences between the direct and indirect vascularization groups were not significant. In the indirect revascularization group, communicating artery patency was confirmed in half of the patients, and 18 of the 21 patients who showed full wound healing within 6 months had a patent communicating artery. Additionally, among the 17 patients who did not show full wound healing within 6 months, 15 had a non-patent communicating artery. As a result, in the indirect vascularization group, it can be seen that identifying the patency of the communicating artery and completing the procedure is beneficial for wound healing.
From a plastic surgeon’s perspective, treating patients with CLI is challenging. Patients often have other comorbidities, and if there is no improvement in blood flow, it is difficult to manage these wounds only with dressings or surgery. Therefore, understanding the angiosome concept and identifying the location of blocked blood vessels is needed, and a systematic consultation with the interventional clinician should be performed.
If surgeons want to preserve a certain vessel for later surgery, they will need to perform an indirect procedure in accordance with this study’s rationale. For example, surgeons planning a flap coverage using a target vessel’s perforator can consult with the physician who conducted the vessel investigation to determine other vessels to be treated in order to avoid the target vessel and increase flap survival rate. In this case, it is thought to be necessary to study whether the flap surgery is likely to succeed in patients with a patent communicating artery.
This study presents some limitations. The authors had a sample size limited to 120 patients and patients were followed up for only 6 months, so any recurrence after 6 months was not considered. Additionally, patients in this study had a poor general health conditions, which could have affected wound status regardless of the blood vessel blockage. It should also be considered that several small collateral vessels could have affected the recovery of wounds, if not necessarily the communicating vessels. However, this part was done by selecting communicating vessels alternatively which can be seen most clearly because small collateral vessels are very difficult to quantify and suggest an end-point during PTA procedure. Finally, this was a retrospective study, which prevents us from establishing causal relationships and limits extrapolation to other populations.
Conclusion
When treating patients with CLI, multiple approaches like wound dressing, managing comorbidities, and revascularization are crucial. It is important to understand the concept of angiosome for vessel revascularization and direct revascularization is recommended. However, if only indirect revascularization can be performed, it is important to ensure the patency of communicating vessels linking the pedal and plantar arterial systems to increase wound healing and decrease the likelihood of wound relapse. Our findings can be useful to explain treatment options or expected progress and outcomes to patients.
Notes
The authors have nothing to disclose.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant founded by the Korean government (MSIT) (2020R1A2C1100891), and was partially supported by the Soonchunhyang University research fund.