Keystone flap for reconstruction of ulnar side defect of the hand: a case report
Article information
Abstract
Soft tissue defects of the hand may present in various forms and are often challenging to treat. The goal of surgical hand reconstruction includes both functional and aesthetic aspects. The keystone-design perforator island flap is a multi-perforator advancement flap with a safe flap harvesting technique, reliable blood supply, minimal donor site morbidity, and a simple dissection process that obviates the need for microsurgical techniques. Our patient was an 85-year-old man with squamous cell carcinoma on the left-hand ulnar side. The patient had difficulty in ambulation and used the affected area of the hand to stand up. Thus, we planned reconstruction using an omega-variant type B keystone flap to further reduce tension during flap insetting and to provide sufficient padding that would protect against excessive pressure postoperatively. The flap and donor site were closed primarily, without any postoperative complications. The patient was satisfied with the outcome after 19-month follow-up.
Introduction
Soft tissue defects of the hand often occur due to trauma, infection, burns, and tumor resection. Skin cancer of the hand may present in a variety of forms and is often challenging to treat. The goal of surgical hand reconstruction includes both functional and aesthetic aspects. Defect coverage is challenging because multi-vector tension forces can affect wounds. In addition, the ulnar side of the hypothenar area is the weight-bearing part of the hand, and adequate wound closure is needed to be stable to withstand pressure.
Keystone-design perforator island flap is a multi-perforator advancement flap that was first reported by Behan in 2003 [1] and is used as an option for reconstruction. This flap has a safe flap harvesting technique, reliable blood supply, minimal donor site morbidity, and a simple dissection process that obviates microsurgical techniques. Since the introduction of the keystone flap (KF), several modifications have been made to effectively reconstruct soft tissue defects of various sizes and shapes.
Herein, we suggest a modified KF method for successfully reconstructing ulnar side defects of the hand caused by skin cancer resection, without causing aesthetic and functional discomfort.
Written informed consent was obtained for publication of this case report and accompanying images.
Case report
An 85-year-old man with squamous cell carcinoma of the ulnar side of his left hand visited our department. Initially, the lesion was diagnosed as an atypical squamous epithelial lesion on a punch biopsy, so we performed excision. After excision, the defect size was 1.5 × 2.5 cm (Fig. 1). The patient had difficulty in ambulation and was accustomed to getting up using the affected area of the hand. Therefore, the area was frequently affected by the patient’s weight. Considering that the affected area would be continuously pressed and rubbed, sufficient padding was required; therefore, flap surgery was selected over skin graft for reconstruction of the defect. We planned reconstruction using omega (Ω) variant type B KF to further reduce tension during flap insetting and to provide sufficient padding to protect against excessive pressure postoperatively. Accordingly, Ω variant type B KF was applied by performing additional rotational movements to further minimize the tension applied to the flap. The flap and donor were closed primarily, without any postoperative complications or injuries of the dorsal cutaneous branch of the ulnar nerve or the branch of the basilic vein. In addition, although the patient was elderly with poor skin elasticity, he did not complain of discomfort associated with severe sagging or tightness of the postoperative skin.
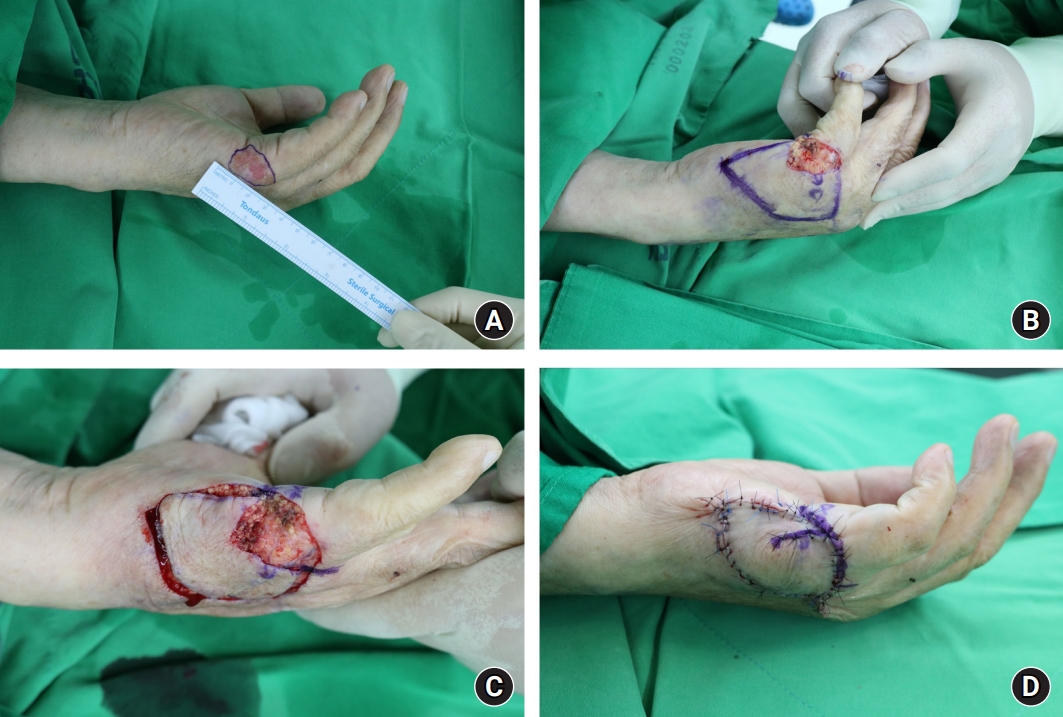
Clinical photographs. (A) A 85-year-old male patient had a skin lesion in the lateral hypothenar area of the left hand. We supposed his lesions to be cancerous and planned an excisional biopsy. (B) After performing excision of the skin lesions, defect size was 1.5 × 2.5 cm2. A 4.0 × 5.5 cm2–sized keystone flap (KF) was designed on the lateral side of the defect. (C) We used the Ω-variant type IIB KF for coverage. (D) The postoperative photograph showed flap insetting with coverage of the dependent portion.
However, the final pathology confirmed the involvement of the distal margin in in situ squamous cell carcinoma. Therefore, an additional skin excision with a safety margin of 4 mm was performed at the distal margin (Fig. 2). Even with an additional small skin defect, sufficient padding could be provided because KF was already performed; thus, we decided to perform a simple skin graft. The skin defect was covered with a full-thickness skin graft, with the wrist as the donor site.

(A) Previous flap site was identified to be a malignant lesion in the pathology examination. We planned further surgical management with a safety margin of 4 mm. (B) After performing further wide excision of the skin lesions, the defect was observed in the previous area of keystone flap (Ω-variant double-arm portion). (C) We used skin graft for coverage of defects to prevent contracture. (D) A postoperative photograph shows the donor site (wrist) in the ipsilateral area.
Finally, the wound healed successfully, and a free margin on the malignant tumor was confirmed. Wound recovery was completed without complications or hand dysfunctions. The patient was satisfied with the outcome after 19-month follow-up, and no cancer recurrence was observed (Fig. 3).
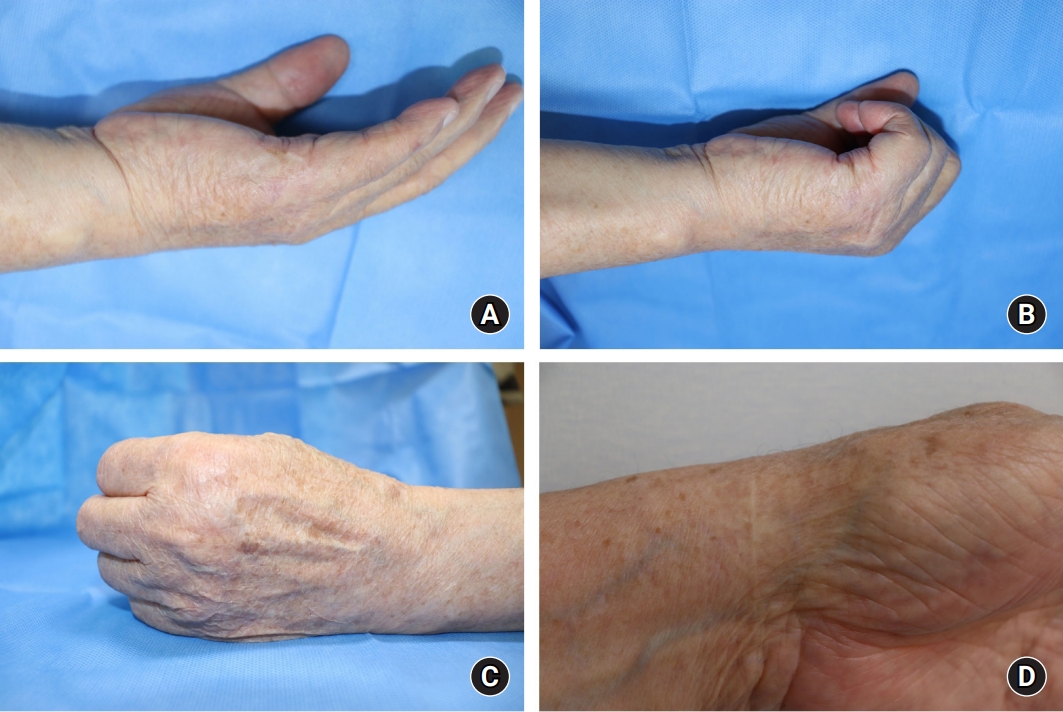
(A) Postoperative photograph after a 19-month follow-up shows satisfactory results and functional outcomes with no contracture of the dependent portion. (B) It was confirmed that motion was not restricted and normal functioning was not hindered. (C) The getting-up position that the patient often assumed showed no discomfort after surgery. (D) The donor site of the graft successfully healed.
Discussion
KF can be used by beginners and experienced surgeons because it is a relatively easy and quick technique. It is also used for the reconstruction of various defects, in most cases in a single stage [2]. KF is clinically used in a variety of anatomical features, including the trunk, limbs, perineum, and head and neck. In particular, when reconstructing a skin cancer defect, it is possible to cover a large defect using only the surrounding tissue without using a separate donor site [3].
Reconstructing hand defects with KF minimizes contracture caused by postoperative scarring and lowers the pliability of the skin, thereby minimizing the dysfunction of the hand [4]. As it is important to apply the proper reconstruction method for each patient, the KF can provide adequate coverage of the area irritated by personal behavioral habits. Thus, the patient can recover satisfactorily without discomfort.
In our case, we considered securing the stability of the flap as the top priority. KF proceeds with dissection by dividing each layer and reducing the tension applied to the flap, as previously described [5,6]. Among modified KFs, the Ω variant type B KF technique has the advantage of additional rotational movement, which further minimizes the tension applied to the flap [7,8].
Although we achieved successful coverage of the dependent portion of the hand defect, our study had limitations. The postoperative pathology of the first surgery was identified as the margin involved. This inevitably required an additional wide excision that involved a portion of the flap. However, this did not affect the survival of the existing flap, and we completed the second surgery using a small full-thickness skin harvested from the ipsilateral wrist. Nevertheless, our case presents an optimal non-microsurgical approach for hand defect reconstruction.
In conclusion, using our selected strategy of the modified KF, we successfully reconstructed the defect in the dependent part of the hand. We suggest that the modified KF is a good option for oncological reconstruction of the hand.
Notes
The authors have nothing to disclose.
Funding
None.
