Hyperbaric oxygen therapy and prostaglandin usage for shred injury of the fingers: a case report
Article information
Abstract
A 53-year-old woman came to the emergency department because her right hand had been stuck in a potato-shredding machine for 30 minutes. The 2nd, 3rd, and 4th fingers were shredded into multiple slices deep into the phalangeal bone, which showed good circulation, and the wounds were cleaned with massive saline irrigation. The slices of each finger were put together to re-form the finger, which was sutured with nylon, and the circulation of the fingers remained good. Three weeks of gentamicin, cefazolin, and hyperbaric oxygen therapy were used for acute traumatic ischemia since color change of the fingers was observed. Six weeks of prostaglandin was used to promote recovery of circulation. The patient was able to grasp with minimal pain and to perform flexion and extension, and the wound completely healed. Radiography showed the bone union process, and digital infrared thermal imaging showed relatively good circulation.
Introduction
Treatment of shred injuries can be challenging for orthopedic hand surgeons. Shred injury is uncommon and can be a surprise for the surgeon. In this case, the injured site had become necrotic, and therefore prostaglandin E1 (PGE1) and hyperbaric oxygen therapy (HBOT) were used, which was different from previously reported shred injury cases. It often requires multiple suture operations, and recurrence of infection and necrosis even after debridement and repair is common. The outcome can be worse if the injury source is contaminated by organic matter [1]. Therefore, the authors present a case report in which the patient underwent several operations to achieve the clinical resolution of such a condition.
Case report
A 53-year-old female patient without any medical history came to the emergency department because her hand had been stuck and was injured severely by a potato-shredding machine. The 1st, 2nd, 3rd, and 4th fingers were inserted into the machine while wearing a glove. The patient came to the emergency room with her right hand inserted into the machine (Fig. 1A-1C). In the operation room, the machine was removed, and the 2nd, 3rd, and 4th finger had been shredded into multiple slices deep into the phalangeal bone. Each sliced part of the shredded finger showed good circulation, and the wounds were cleaned with massive saline irrigation (Fig. 1D, 1E). The slices of each finger were put together to form the finger, and it was sutured with 4-0 and 5-0 nylon. After suturing all fingers, the circulation of the fingers was good (Fig. 2).

A 53-year-old female patient injured her 1st to 4th fingers in a shredding machine. (A) The 1st to 4th fingers were inserted into the machine. (B) Initial X-ray with the machine. (C) Initial three-dimensional computed tomography with the machine. (D, E) After machine removal and massive irrigation; the 2nd, 3rd, and 4th fingers in the (D) dorsal aspect and (E) volar aspect.

After debridement and suturing. (A) Plantar aspect. (B) Dorsal aspect. (C) Fingertips. (D) X-ray images at postoperative 2 weeks; anteroposterior, oblique, and lateral. (E) Postoperative computed tomography, which shows multiple simple fractures at the right 1st, 2nd, 3rd, and 4th distal phalanges and the 3rd middle phalanx without displacement.
The direction of the shred injury was initially sagittal and most of the volar aspect was intact; however, a portion of the distal fingers showed complete detachment. Nevertheless, during surgery, we have identified only partial damage to the arterial branches, and therefore blood flow problems were expected to be low. Consequently, HBOT and prostaglandin (PG) treatment were not planned, but on postoperative day (POD) 1 ischemic change, such as discoloration and darkening, was observed on 2nd and 3rd fingers, whereas 4th finger showed slight color change. According to the 14 criteria of Undersea and Hyperbaric Medical Society, the wound was defined as ‘other acute traumatic ischemia,’ and therefore HBOT and PG were started. The treatment was repeated until color change improvement was observed, and a total of 24 cycles were completed. For each treatment period, 2 hours and 10 minutes of 2.4 atmospheres absolute was carried out [2]. Four weeks of intravenous PGE1 and 2 weeks of per-oral PGI2 were done for circulation recovery of fingertips [3,4].
Total 3 weeks of aminoglycoside antibiotics (gentamicin), and 3 and 1/2 weeks of 1st generation cephalosporin (cefazolin) were used for open fracture [5]. Range of finger motion exercises were started from 1 week after surgery by removing the dorsal functional splint for early exercise and circulation [6]. After 2 weeks of daily dressing with hydrocolloid gauze (Physiotulle, Coloplast, Humlebæk, Denmark), recombinant human epidermal growth factor ointment (Easy-EF, CGBIO, Seoul, Korea) [7], and ofloxacin antibiotic ointment (Ocuflox, Samil Co., Ltd., Seoul, Korea) [8], total stitch out was done 2 weeks after surgery (Fig. 3A). Then, the second debridement and suture were completed for wound dehiscence on the 2nd and 3rd distal phalanges (Fig. 3B, 3C).

(A) Wound dehiscence on the distal phalanx of the 3rd finger. (B) Second debridement and suturing of the distal phalanx of the 3rd finger. (C) After the second debridement and suturing.
Daily dressing was done for 2 weeks after the second debridement for the 2nd and 3rd fingers. Two weeks after the second operation, additional debridement was done for necrotic skin tissue on the radial aspect of the 3rd fingertip. The patient was transferred out to the physical medicine and rehabilitation department for functional movement and rehabilitation. After the final operation, there were no signs of infection, there was a steady decrease in the erythrocyte sedimentation rate and C-reactive protein, and physical signs improved.
At POD 3 months, the right hand showed an overall Poor to Fair + grade on the Manual Muscle Test. Although there was a gradual muscle increase, all fingers showed muscle weakness of the distal interphalangeal (DIP) joint flexor-extensor.
At POD 4 months, pain was observed at the right hand end range. Partial range of motion (ROM) recovery of the patient’s thumb proximal interphalangeal (PIP) joint extension, 2nd finger PIP extension, 3rd finger PIP flexion, 4th finger PIP flexion, 2nd finger DIP flexion, and 3rd finger DIP extension was observed. According to Korea-Modified Barthel Index, the patient had a similar performance level of independent daily activities. However, the patient required more time or assistance when performing two-handed activities such as taking a bath or dressing. On the Jebsen-Taylor Hand Function Test, difficulty of pinching and grasping small objects was observed on the right thumb to 2nd fingertip. The used of thumb and 5th finger was observed when grasping small objects.
At POD 6 months, sensitivity of the right hand was improved (as on POD 4 months, patient showed sensitivity and pain when touching the goniometer, but at 6 months, pain sensitivity had been adjusted). On the passive and active ROM results, ROM was partially improved of the 2nd finger metacarpophalangeal (MP), PIP, DIP joint flexion, 3rd finger MP, DIP, PIP joint flexion, 4th finger PIP, DIP joint flexion, 5th finger PIP, DIP joint flexion.
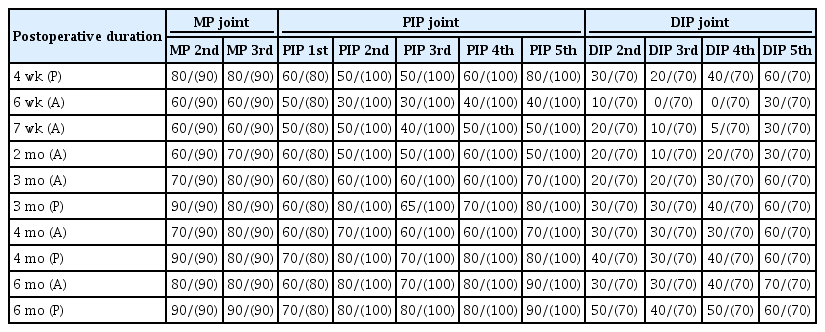
During this period, the patient was able to grasp with minimal pain and do flexion and extension (Table 1, which shows continuous finger ROM improvement until POD 6 months) (Fig. 4), and the wound was completely healed (Fig. 5). Radiography showed bony union process, and a digital infrared thermal imaging test showed that circulation was relatively good (Fig. 6).

(A) The wound was fully healed; new fingernails grew at postoperative 8 weeks. Active range of motion (ROM) at postoperative 8 weeks. (B) Active ROM on postoperative 6 months.

Wound healing process of the volar aspect of the right 2nd and 3rd fingers from the day of trauma to postoperative 6 months. Ischemia and necrosis all normalized over time. POD, postoperative day.
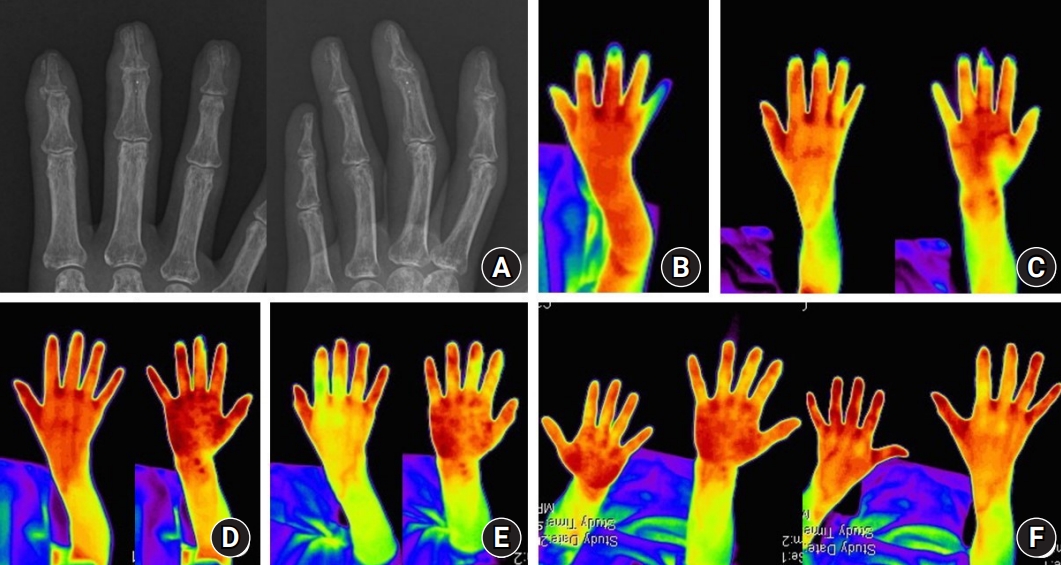
(A) X-ray images at postoperative 3 months, which show that the complete fractures at the 2nd to 4th distal phalanges and the 3rd middle phalanges are in the healing process. (B) The result of digital infrared thermal imaging (DITI) at postoperative 2 weeks. Infrared shows temperature difference between distal and proximal parts of the dorsal aspect of the right 3rd finger (temperature difference, 2.58°C). Infrared shows the temperature difference between the distal and proximal parts of the volar aspect of the right 3rd finger (temperature difference, 2.54°C). These findings are suggestive of a circulation defect in the distal part of the dorsal and volar aspects of the right 3rd finger compared to the proximal part. (C) DITI at postoperative 3 weeks. Infrared shows the temperature difference between the distal and proximal parts of the dorsal aspect of the right 3rd finger (temperature difference, 2.00°C). Infrared shows the temperature difference between the distal and proximal parts of the volar aspect of the right 3rd finger (temperature difference, 3.67°C). These findings are suggestive of improvement of the circulation defect in the distal part of dorsum and aggravation of the circulation defect in the volar aspect of the right 3rd finger compared to the proximal part. (D) DITI at postoperative 5 weeks. Infrared shows the temperature difference between the distal and proximal parts of the volar aspect of the right 3rd finger (temperature difference, 1.33°C). These findings are suggestive of a circulation defect in the distal part of the dorsal and volar aspects of the right 3rd finger compared to the proximal part (up to normal level). (E) DITI at postoperative 2 months. Infrared shows an higher temperature in the distal part than in the proximal part of the dorsal aspect of the right 2nd, 3rd fingers and the volar aspect of the right 3rd finger. These findings are suggestive of neovascularization of end arteries on the dorsal side of the 2nd, 3rd fingers, and the volar side of the 3rd finger. (F) DITI at postoperative 6 months. The temperature difference of the 2nd, 3rd, and 4th injured fingers was less than 1°C, indicating complete revascularization. There is no evidence of a circulation defect or complex regional pain syndrome.
Written informed consent was obtained for publication of this case report and accompanying images.
Discussion
Shred injury is a critical injury to the hand as circulation recovery is difficult to be achieved. Fortunately, in this case, the finger was shredded vertically, which minimized the damage to most arteries and nerves, allowing recovery of circulation. Nevertheless, on POD 1, acute traumatic ischemia was noted as color change at 2nd, 3rd, 4th fingertips were observed and therefore HBOT was initiated. Although blood circulation of the injured site was confirmed at the surgical table, we chose to treat the patient with PGE1 and HBOT as there was no guarantee that good circulation status would be preserved, and reversal of the wound would be difficult once the wound becomes necrotic.
The effect of PGE1 is a drug delivery system through antiplatelet effects and vasodilation [9]. The mechanism of HBOT is the main rationalization for using it in crush injuries and compartment syndromes. One, HBOT increases oxygen availability in the hypoxic tissues in the early recovery period when perfusion is low. Two, HBOT supplements tissue oxygen tensions to enable the host to respond. Adequate oxygen can be diffused in plasma under HBOT condition to avoid hemoglobin-borne oxygen and keep the tissues alive. An increased tissue oxygen tension results in a three-fold “driving force” for oxygen to dissolve through tissue fluids. This helps to counterbalance the hypoxia developing from the increased oxygen diffusion distance from the capillary to the cell through the surrounding edema [10].
Side effects of HBOT are barotrauma, acute central nervous system oxygen toxicity, reversible myopia and clouding of preexisting cataracts and contraindications include untreated pneumothorax, and more. The above contraindications were not applicable to our patient and no side effects were noted.
We encourage early ROM exercise and physical therapy; however, the patient showed low compliance, as she was sensitive to pain until POD 8 weeks. Pain subsided over the duration of POD 6months. All soft tissue was recovered with very minimal remaining pain as well as intact sensory function. In the end, we gained significant motor and sensory function recovery.
In our case, the hand was cut clearly sagittal, and minimal displacement was observed on postoperative X-ray. Hence, we continued with conservative management. At the moment, soft tissue healing is complete.
Notes
The authors have nothing to disclose.
Acknowledgements
We would like to thank our advisor Dr. Yoonsuk Lee, from Departments of Emergency Medicine, Yonsei University Wonju College of Medicine, who has been an invaluable mentor. His gift for conceptualization, his enduring encouragement, and his practical advice have been an inestimable source of support for us during this process. We would also like to thank for his advice and feedback. His varied perspectives have helped us to strengthen our work.
Notes
Funding
None.