Distribution of Anterolateral Thigh Flap Perforator Vessels and Its Clinical Applications in Malaysian Population
Article information
Abstract
Purpose
Extensive studies regarding vascular anatomy and clinical applications of anterolateral thigh (ALT) flap has been conducted for many years. However, the ALT flap perforator vessels anatomy in the Malaysian population is not well-analyzed. The purpose of this study was to determine the distribution of ALT flap perforator vessels and its clinical applications in reconstructive surgery.
Methods
This is a retrospective cross-sectional study conducted in two main centers of reconstructive surgery. A total of 142 cases of ALT flaps that used as an option for soft tissue reconstruction was selected. Vascular anatomy of ALT flaps was studied precisely including the origin of vessels, location of perforators, and types of perforator vessels intraoperatively during the flap harvest.
Results
The distribution of ALT flap perforator vessels can be found at three specific locations on the thigh namely perforators A, B, and C. The highest number of cutaneous perforator vessels that supplied the ALT flap was musculocutaneous perforator with 72.3%, and dominantly at perforators B and C. The remaining perforator vessels were septocutaneous perforator with 27.7%, presented mainly at perforator A. A majority of cases involved the reconstruction of wound defects following tumor resection and trauma. The most area of reconstruction was the lower limb with 33.8%.
Conclusion
The distribution of ALT flap perforator vessels can be predicted during flap harvest and can be applied in numerous clinical applications for wound defect coverage. The knowledge regarding vascular anatomy of ALT flap perforator vessels can aid plastic surgeons in reconstructive surgery.
INTRODUCTION
In the last few decades, exposure and introduction of microsurgery and improvement in microsurgical techniques with the understanding of perforator flaps in reconstructive surgery have gained much interest in seeking better free flaps for soft tissue coverage regardless of simple or complicated defects. An ultimate reconstruction surgery preserves both function and aesthetic appearances not only toward the defect area but also the donor area without compromising the outcome of the surgery.
The anterolateral thigh (ALT) flap was described in 1984 [1] as a septocutaneous perforator flap, based on the descending branch of the lateral circumflex femoral artery (LCFA) [2]. Subsequently, it was found that a significant number of perforator vessels could be identified as musculocutaneous perforators. Existing data showed that the perforator vessels supplying the ALT flap were mainly originated from the descending branch of the LCFA. However, they could originate from vessels other than the descending branch of the LCFA [3-7]. It is reported, the variation of origin vessel for the perforator vessels could be from the transverse branch of the LCFA, oblique branch of the LCFA, directly from the LCFA, and the common femoral artery [6]. Thus, the untoward aspects of the ALT flap are the complexity and variation of its vasculature that might complicate during flap harvest. Despite the variation of its origin, the dominant perforator vessels supply to the ALT was found abundantly in the center of the ALT [2,4,8-10].
The simple ABC system is reliable in predicting the perforator vessel location during harvesting and dissecting the flap. According to this system, once locating the perforator B is done, which is the most consistent location at the midpoint of the line connecting the anterior superior iliac spine (ASIS) and superolateral corner of patella, perforators A and C easily be found approximately 5 cm away from perforator B proximal (A) and distal (C), respectively [11,12].
The ALT flap is a popular choice because of its favorable characteristics that make it ideal for clinical application in reconstructive surgery [13]. It is a reliable, versatile flap not only for soft tissue coverage after oncological resection surgery procedure but also for managing various other injuries [14]. Clinical applications of the ALT flap are broad and described extensively as a beneficial choice of the flap in head and neck, upper and lower extremity, trunk, breast, and abdomen [15-17]. It can be harvested faster, with little or minimal donor site morbidity. The donor site contains numerous soft tissues and can be tailored accordingly for example fasciocutaneous, myocutaneous, and chimeric flaps depend on the wound defects [18-21]. Furthermore, it also provides long pedicle length with good diameter that helps in complex reconstruction [22]. This study was a frontier of knowledge in determining the distribution of ALT flap perforator vessels and its clinical applications among the Malaysian population. This information can be used as a guide to facilitate plastic surgeons in planning and dissecting the flap.
MATERIALS AND METHODS
This is a cross-sectional study involving 142 patients who underwent reconstructive surgery with ALT flap under the Reconstructive Sciences Unit, Hospital Universiti Sains Malaysia and the Department of Plastic and Reconstructive Surgery, Hospital Kuala Lumpur, from 2007 until 2019. Data were obtained from the patients’ case and operative notes. It included patients’ demographics, indications for surgery, area of reconstruction, type of the ALT flap, dimensions of the flap, and perforator vessels distribution. The conduct of this study was approved by the Human Research Ethics Committee of Universiti Sains Malaysia (USM/JEPeM/18010080) and Medical Research & Ethics Committee (MREC), Ministry of Health Malaysia (NMMR-18-552-40522). The informed consent was waived.
1. Surgical operative procedure
The flap was harvested according to the standard procedure mentioned in the literature. In markings for the ALT flap, it was marked based on the perforator vessels that supplied the skin territory of the flap detected by hand-held Doppler ultrasound. Important landmarks for the flap include the ASIS and the superior lateral border of the patella. The flap was centered at the midpoint of a longitudinal line drawn between these two landmarks. A circle of 3-cm radius defined the area at which the perforator vessels, either septocutaneous or musculocutaneous, exit. The skin paddle was then designed around the marked perforator vessels. Skin and subcutaneous tissue were then gently dissected to enter into the intermuscular septum between rectus femoris and vastus lateralis muscles using surgical loupe. The rectus femoris muscle was retracted to expose the descending branch of the LCFA. Once the artery was identified, a search is made for either the septocutaneous perforator or the musculocutaneous perforator as the dominant perforator vessels. The perforators were then dissected along the main pedicle and skin paddle was incised after freeing the pedicle. All the relevant findings required were documented in ALT proforma.
2. Data and statistical analysis
The frequency data were presented in numbers, percentages, and mean±standard deviation. Further analysis was made regarding numbers of perforator vessel and type of perforators (septocutaneous or musculocutaneous) with the location of the thigh.
RESULTS
1. Patients demographics
The majority of patients were in the age group of 11 to 20 years old (n=27, 19.0%). The age range of the patients was 2 to 71 years, with a mean age of 34.80±19 years old. Patients were predominantly male (n=115, 81.0%) and Malay (n=125, 88.0%). Most of the patients were nonsmokers (n=104, 73.2%). One hundred and 30 patients (91.5%) were nondiabetics and 104 (73.2%) were nonhypertensive.
2. Anatomical distribution of anterolateral thigh flap perforator vessels
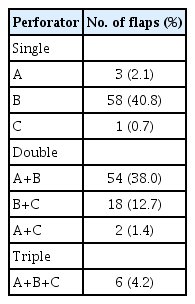
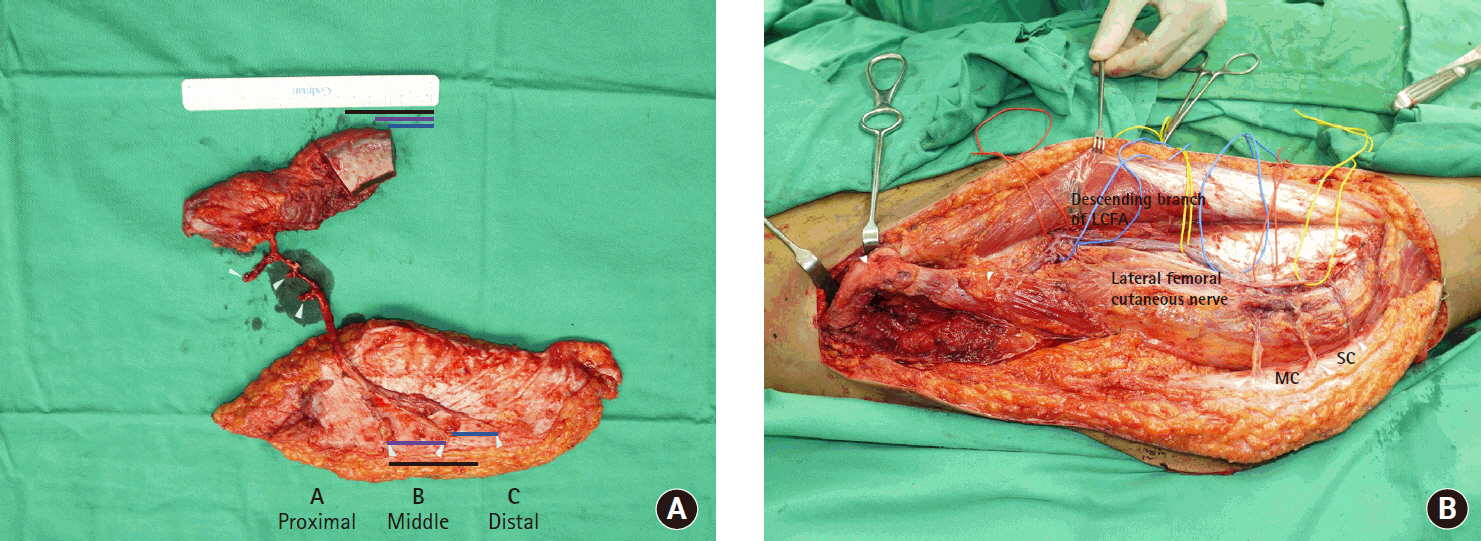
Table 1 summarizes the presence of the ALT perforator vessels based on their location of the thigh. Each flap could have cutaneous perforators presented as one to three areas according to the location of the thigh intraoperatively. The presence of cutaneous perforator vessels was identified either as perforator A (proximal), perforator B (middle), or perforator C (distal). Approximately 60% of the total flap cutaneous perforator vessels could be identified in more than one location. When the perforator vessels were present in only one location (43.7%), most of them could be identified in perforator B (middle) with 58 cases (40.8%), followed by perforator A (proximal) with three cases (2.1%) and perforator C (distal) with one case (0.7%). For cutaneous perforator vessels that were present in two locations of the thigh, most of them could be identified at perforators A and B with 54 cases (38.0%), followed perforator B and C with 18 cases (12.7%) and perforator A and C with two cases (1.4%). Only in six cases (4.2%) cutaneous perforator vessels were present in all three locations of the thigh. There was one case of ALT flap with perforator vessels located at the distal part of the thigh (C). The pedicle length of this flap was 15 cm from the descending branch of the LCFA with a skin paddle sized 14×28 cm. Table 2 shows a total of 347 perforator vessels in 142 cases of ALT flap. The perforator vessels could be divided into septocutaneous and musculocutaneous. Besides, the presence of perforator vessels could be classified according to their location on their thigh, that is, either proximal (A), middle (B), or distal (C) (Fig. 1). Most perforator vessels were located at the middle thigh (B) with 239 perforator vessels (68.9%). This is followed by proximal thigh (A) with 71 perforator vessels (20.5%) and distal thigh (C) with 37 perforator vessels (10.7%). Musculocutaneous perforators were the most perforator vessels identified with 251 perforators (72.3%) and located mostly at the middle thigh (B). There were 96 septocutaneous perforators (27.7%) mostly identified at the proximal thigh (A).
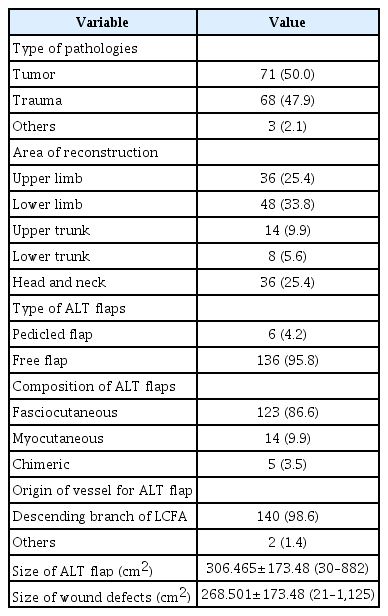
3. Types of anterolateral thigh flap, indications and reconstructed areas
A majority of cases involved the reconstruction of the defected areas following tumor resection with 71 cases (50.0%), followed by trauma with 68 cases (47.9%) and others with three cases (2.1%). Cases in other categories include infection and vascular malformation. The most common region or area of reconstruction using ALT flap was the lower limb with 48 cases (33.8%), followed by upper limb and head and neck areas with 36 cases (25.4%), upper trunk with 14 cases (9.9%), and lower trunk with eight cases (5.6%). Most ALT flaps were harvested as free flaps with 136 cases (95.8%). Six cases (4.2%) were pedicled flap. Out of 142 cases, 140 cases (98.6%) were of ALT flap supplied by the descending branch of the LCFA. The remaining two cases (1.4%) were supplied by the transverse branch of the LCFA. The ALT flaps were mainly harvested as fasciocutaneous flaps in 123 cases (86.6%), followed by myocutaneous flaps in 14 cases (9.9%) and chimeric flap in remaining five cases (3.5%). The mean size of the harvested ALT flap was 306.5±173.5 cm2 and the mean of the wound defect size was 268.5±173.5 cm2. The overall clinical application and reconstruction are summarized in Table 3.
DISCUSSION
Microvascular flap surgery has become an important part of reconstructive surgery for the last few decades as it facilitates the closure of various types of tissue defects. A wide range of free flaps has become available for resurfacing simple and complicated defects. The ALT flap as described fulfills most criteria as an ideal flap to be a ‘workhorse’ flap for soft tissue reconstruction. It was earlier recognized as septocutaneous perforator-based flap and has gained its popularity since then because of its vast advantages [1]. It was based on perforator vessels derived from the lateral circumflex femoral arterial system. Later, several authors have thoroughly investigated the anatomy of perforating vessels and found that in most cases, the flap was supplied by musculocutaneous perforator vessels instead of septocutaneous perforator vessels [3-7].
The qualities of ideal soft tissue coverage with free flaps consist of (1) versatility in design with sufficient tissue coverage, (2) superior texture, (3) low morbidity of the donor site, (4) availability of diverse tissue types on one pedicle, (5) potential for reinnervation, large and long pedicle, (6) feasibility of the two-team approach, and (7) importantly, consistent anatomy for a feasible and safe flap dissection. Thus, the ALT flap meets all the above criteria mentioned as a ‘workhorse’ flap. One of the disadvantages of the ALT flap is the complexity and variations of its vasculatures. Failure to understand its variability can lead to tissue loss [23]. Despite the variations of their origin, the dominant perforator vessels supply to the ALT flap was from the descending branch of the LCFA, and a majority of the perforator vessels were found in the middle of thigh [4]. The location of cutaneous perforators can be found in predictable locations on the thigh. They can be classified as perforator A (proximal), perforator B (middle), and perforator C (distal). Flap design and marking of the cutaneous perforators using hand-held Doppler based on its location on the thigh will assist further in identifying the perforators during flap harvest. This ABC system classification by Yu et al. [11,12] seems very helpful in identifying cutaneous perforator intraoperatively.
In this study, among 142 successfully raised ALT flaps, the pedicle of ALT flap originated mainly from the descending branch of the LCFA. Only one flap has the pedicle originated from the transverse branch of LCFA. Thus, despite the variation in anatomical origins of the ALT flap, it still can be harvested successfully based on the descending branch of and the transverse branch of LCFA.
The presence of cutaneous perforator vessels according to the location of the thigh (A,B, and C) were identified. Sixty-two ALT flaps perforator vessels (43.7%) were present at one location only, that is, either A, B, or C. Seventy-four ALT flaps perforator vessels (52.1%) were present at two locations of the thigh, either A+B, B+C, or A+C and six ALT flaps perforator vessels (4.2%) presence at all three location thigh. The presence of cutaneous perforator vessels reported in this study predominantly involved two locations of the thigh, which is in line with previous studies [11,12].
The highest number of cutaneous perforator vessels that supply the ALT flap were the musculocutaneous perforators with 72.3% and dominantly at perforators B and C. The remaining perforator vessels were septocutaneous perforator and presented mainly at perforator A. In general, the proximal perforator vessels have high chance to be septocutaneous perforator, whereas middle and distal parts of thigh perforator vessels were usually the musculocutaneous perforator. These findings on the distribution of ALT perforator vessels and type of cutaneous perforators are similar to those reported in previous studies [2,4,8-10]. Among the 142 ALT flaps, there was one case of ALT flap with perforator vessels located at the distal part of the thigh (C). The pedicle length of this flap was 15 cm from the descending branch of the LCFA with a skin paddle sized 14×28 cm. This flap was successfully harvested and employed onto the wound defect.
ALT flap is a reliable versatile flap for soft tissue coverage for various wound defects. Clinical applications of ALT flap are broad and have been described extensively as the beneficial choice of flap postresection surgeries and also wound defects in traumatic injuries involving any region of the body [14-16]. In this study, the ALT flap was widely used as an option for soft tissue reconstruction following tumor resection (50.0%) and trauma injuries (47.9%). In about 3% of cases, ALT flap was used as a choice in other types of pathologies for example infection and vascular malformations. Thus, the ALT flap is an ideal flap in view of its versatility and reliability as a choice for soft tissue coverage.
CONCLUSION
The distribution of ALT flap perforator vessels in the Malaysian population can be predicted during flap marking and harvest by applying the ABC system. The knowledge regarding the vascular anatomy of the ALT flap can facilitate plastic surgeons to harvest the flap successfully by understanding the distribution of perforator vessels. The ALT flap has numerous advantages in clinical applications which can be an ideal flap for soft tissue coverage in various types of wound defects. Thus, it is advocated that the ALT flap can be reliable and safe to be employed as a ‘workhorse’ flap in the field of reconstructive surgery.
Notes
The authors have nothing to disclose.
Acknowledgements
The authors would like to acknowledge those who contributed to this study, directly or indirectly from Hospital Universiti Sains Malaysia and Hospital Kuala Lumpur.