|
 |
- Search
| Arch Hand Microsurg > Volume 25(3); 2020 > Article |
|
Abstract
Purpose
Distal radius fractures (DRFs) are often observed in simple trauma in older women with osteoporosis, and severe trauma caused by traffic or fall accidents. In this study, we aim to classify the DRFs according to injury mechanism, and statistically compare epidemiologic factors, radiological characteristics, and functional scores.
Methods
From 2013 to 2018, 112 cases of trauma in 104 patients (70 monotraumas and 42 severe traumas) diagnosed with DRFs were included. Patients were divided into the low-energy monotrauma (ML), high-energy monotrauma (MH), and severe trauma groups and analyzed for differences in sex, Injury Severity Score (ISS), accompanying ipsilateral injuries, radiologic indices, AO/OTA classification, and functional outcome scores (disabilities of the arm, shoulder, and hand [DASH] and Modified Mayo Wrist Score).
Results
Significant differences were observed in sex, age, ISS, and accompanying ipsilateral injury among three group (p<0.001). Distribution of AO classification was not significantly different among the groups. Especially, sex, age, and accompanying ipsilateral injury were significantly different between the ML and MH groups (p<0.001). Postoperative DASH and MMWS were significantly different between the monotrauma and severe trauma groups (p<0.001).
Conclusion
Severe trauma with DRFs was observed at a lower age and more frequently accompanied by ipsilateral injury and high ISS. Additionally, the functional outcomes were lower after severe trauma than after monotrauma. Therefore, for DRF patients with severe trauma, attention should be paid to the pattern of fracture as well as the accompanying injury and postoperative management and rehabilitation associated with it.
Distal radius fractures (DRFs) are the most common fractures of the upper extremity, and various treatments for DRFs have been reported; however, options for DRFs due to trauma energy are seldom reported. DRFs may be sustained due to three types of trauma energy. First, it is often the result of a low-energy trauma, which is a simple injury encountered when a person lands on his/her wrist extended; in particular, elderly women with reduced bone density will have complex fractures even with simple trauma caused by lower-energy injuries [1-3]. Second, high-energy injuries occur only in the upper extremity due to events such as car accidents; this is simple trauma that is not accompanied by any severe trauma (ST) in other areas; however, DRFs can occur as complex fractures due to their high-energy trauma [2,4]. Third, DRFs can occur after ST, which is accompanied by multiple organ injuries due to high-energy trauma. In this case, depending on the degree of high-energy injury affecting the upper extremity, both simple and complex fractures can occur. This ST is accompanied by damages to the brain, lung, liver, and intestines, which are related to life support, or by open, pelvic, and multiple fractures that are related to orthopedically severe damage to soft tissues. In particular, if these patients with ST miss appropriate surgery time or are unconscious, it may affect their future rehabilitation. In South Korea, trauma centers have been established to provide specialized treatment only to such ST patients.
This study aimed to evaluate and compare the epidemiologic features of ST patients with those of monotrauma patients with DRF. We categorized DRF patients according to the types of trauma. Subsequently, we compared the radiological features and functional results between the ST group and the monotrauma group.
Emergency medical centers in South Korea are subdivided into the regional emergency center, local emergency medical centers, and local emergency medical institutions. The regional trauma center is dedicated to ST. This study focused on patients who visited the Pusan National University Hospital, designated as a regional medical center and a regional trauma center. The study was approved by the Institutional Review Board of Pusan National University Hospital (No. H-1906-030-080).
Patients who visited the emergency center of Pusan National University Hospital from December 2013 to July 2018, were aged ≥20 years, were diagnosed with DRF and underwent surgical treatment were initially included. Of the 109 enrolled patients (119 cases), five patients (7 cases) were lost to follow-up. Finally, 104 patients (112 cases) were included. Among the 104 patients, the evaluation of the disabilities of the arm, shoulder, and hand (DASH) score was not performed in five patients (5 cases) and a telephone survey was performed in five patients (5 cases).
We first classified patients into two groups according to the Injury Severity Score (ISS). The ISS is an established medical score that assesses trauma severity and used to define the term major trauma. It correlates with mortality, morbidity, and hospitalization time after trauma [5]. Multiple injuries are scored using the Abbreviated Injury Scale (AIS) according to six body regions. The ISS score is the sum of squares of the highest AIS grades in each of the three most severely injured body regions (Table 1).
ST patients were defined as those with DRFs and an ISS of ≥16. Of the 112 cases, 42 cases were of ST. Monotrauma patients were defined as those with isolated DRFs or those with DRFs and fractures at other body parts and with an ISS of <16. These patients were further categorized into low-energy monotrauma (ML) and high-energy monotrauma (MH) according to the definition of MH [6]. The criteria for high-energy trauma are as follows [6]: a fall from >3 m, a car accident velocity of >60 km/hr, a motorcycle accident velocity of >30 km/hr, vehicle shortening of >50 cm, vehicle depression of the passenger side of >30 cm, vehicle rollover of passenger thrown from the vehicle, fatality in the same vehicle, and car or motorcycle versus pedestrian or bicyclist velocity of >10 km/hr. Additionally, it was classified as MH due to compression and crushing injury caused by a machine (Fig. 1).
Only one surgeon performed surgical treatment for all patients. Surgical techniques used with a volar plate or Kirschner wire (K-wire) fixation with/without bone graft. K-wire fixation was used for simple and extra-articular fractures and bone graft was used for severe fragmented intra-articular fractures.
All patients were evaluated for differences in sex, ISS, accompanying ipsilateral injury, and surgical method according to the medical chart. We assessed the radiological indices and AO/OTA classification using radiological images at initial trauma and immediately after surgery. Radiologic indices included volar tilt angle, radial inclination, and ulnar variance using the project-a-line technique. The ipsilateral injury was defined as the existence of a fracture at the ipsilateral extremity. To evaluate the functional results, we accessed the DASH questionnaire and calculated the Modified Mayo Wrist Score (MMWS) at 1 year after surgery.
For statistical analysis of radiological indices and functional outcomes, one-way analysis of variance and Pearson chi-squared test were used. The post-hoc test using the Bonferroni method was used to evaluate significant differences between the groups. The statistical significance level was set at p<0.05.
Of the total of 104 patients (112 cases) included in this study, 53 and 51 were females and males, respectively. The mode of injury was car accidents in 25 cases, fall accidents in 39 cases, and slip accidents in 45 cases. Furthermore, there was one case each of crush damage, rope wrapped accident during work, and stab wounds (Fig. 2).
Of the 112 cases, 51 were in the ML group, 19 in the MH group, and 42 in the ST group. By sex, males accounted for 29.4%, 84.2%, and 66.7% of all patients in the ML, MH, and ST groups, respectively (Table 2). The mean patient age was 64, 47, and 51 years in the ML, MH, and ST groups, respectively. Both sex and age were not significantly different between the MH and ST groups which included patients with injuries due to MH trauma (p=0.052, p=0.979), but they were significantly different between the ML and MH groups and between the ML and ST groups (p<0.001) (Table 3).
The ISS was 5.08±2.01, 7.74±3.66, and 26.79±9.8 in the ML, MH, and ST groups, respectively (Table 2). The difference in trauma energy between the monotrauma and ST groups was significant (p<0.0001), whereas within the monotrauma groups was not significant (p=0.365) (Table 3).
The time from injury to surgery was 8.9, 7.9, and 12.1 days in the ML, MH, and ST groups, respectively. The difference in the time from injury to surgery among the three groups was not significant (p=0.130).
Two patients in the ST group required revision surgery because reduction loss was observed owing to patient incorporation. One patient had a brain injury and another had a psychological problem. All patients underwent bone union at the final follow-up.
Patients who underwent only volar plate fixation after injury accounted for 98.0%, 84.2%, and 97.6% in the ML, MH, and ST groups, respectively (Table 2), showing a significant difference (p=0.032) between the ML and ST groups (p=0.009), and between the ML and MH groups (p=0.02) (Table 3). Whether using K-wire fixation or bone graft, the difference was not significant in the three groups (p≥0.05).
The incidence of ipsilateral injury was 5.9%, 42.1%, and 64.3% in the ML, MH, and ST groups, respectively. The post-hoc test revealed a significant difference between the ML and MH groups and between the ML and ST groups (p<0.0001), but not between the MH and ST groups, which included patients with injuries due to MH (p=0.105).
The results of the radiological examination conducted before and after surgery showed no significant differences, except the fracture site gap that was significantly different between the monotrauma and ST groups (p<0.001), but not between the ML and MH groups (p>0.999).
All patients underwent bone union at the last follow-up. None of the patients required revision surgery.
The results of DASH and MMWS to evaluate functional outcomes showed significant differences in all groups (p<0.001). As the energy of the mechanism of injury increased, functional outcomes worsened (Tables 3, 4). The distribution of AO/OTA Classification did not show significant differences (p=0.25), but the predominance of type C was identified in the MH and ST groups (Table 2).
There are several classification systems for DRFs, but it is difficult to classify fractures according to trauma energy [6]. Few papers have compared and analyzed the results by classifying DRFs according to the degree of trauma energy [2,4,6]. We can expect easily that patients with high-energy trauma will have a higher rate of complex fractures than those with low-energy trauma, which subsequently results in worse functional outcomes. However, previous studies have reported no correlation between the extent of trauma and AO/OTA classification [7]. This is due to the involvement of various factors, including osteoporosis, concomitant injuries, the degree of external trauma, and the mechanism [1-3]. Therefore, we classified the clinical characteristics of each group by dividing them into three groups based on the injury mechanism. Subsequently, we analyzed the radiological findings, types of fractures, and functional outcomes in patients after surgery.
The ST and MH groups mostly included young and male patients among the three groups. According to the injury mechanism, high-energy trauma such as fall or traffic accidents was the main injury mechanism in the ST and MH groups (Fig. 2). Relatively, slip down is the most common injury mechanism, and most of the patients included in the ML group were postmenopausal women with decreasing bone density. Moreover, there might be a selection bias because our study was conducted in a tertiary university hospital where patients with simple fractures do not usually visit. In this study, although the statistical significance of simple trauma was not high, there were several cases of complex fractures in simple trauma. This is considered a feature of the ML group that comprised several elderly patients with osteoporosis. In previous studies assessing DRFs in patients with high-energy trauma [6,8], there were several complex articular fracture types and high ipsilateral damages in the high-energy group. In this study, the same result was observed, that is the accompanying ipsilateral injury was high, but there was no statistical significance for the type of fracture. Additionally, the accompanying rate of hand injuries among ST patients was 3.6%, and the concomitant injury was a significant factor affecting the functional outcomes after treatment. This result is probably due to the high-energy injury in the ST group, which likely causes other injuries to the affected area.
We expected that the MH and ST groups would have poor results in terms of radiological indices than the ML group; however, the actual statistical analysis results showed no significant difference. The preoperative and postoperative radiological indices did not show any difference between the three groups. Most of the patients in the MH and ST groups are young men; thus, performing union in the fracture site is considered advantageous in these young patients, which might affect statistical results. Additionally, due to the recent development of surgical techniques and tools and equipment, types of fracture do not seem to affect radiological parameters [9]. There was no significant difference in the preoperative radiological parameters among the three groups. This indicates that simple slip down might cause a complex fracture because several elderly women were likely to have osteoporosis in the ML group.
In a previous study that compared patients with isolated fractures and those with polytrauma, there were no significant differences between the groups in terms of union, but the overall results were significantly lower in patients with polytrauma than in patients with isolated fractures in terms of functional outcomes [4,10]. Although no statistical difference in radiological indices was observed among the groups, poor functional outcomes were observed in the MH and ST groups. We hypothesized that this is due to the high ISS and accompanying injuries. In our experience, patients in the ST group have poor cooperation due to polytrauma, which lead to difficulty in diagnosing and treating these patients. In this study, the time from injury to surgery was longer in the ST group than that in the ML group. In the ML group, 90.2% of patients underwent surgery within 10 days from injury. Moreover, 36.8% and 45.2% of patients in the MH and ST groups, respectively, underwent surgery after >10 days from the injury date. In particular, all four patients in the ML group who underwent surgery after 3 weeks were all operated due to reduction loss during conservative treatment. In ST patients with accompanying polytrauma, surgery related to vital signs, such as thoracic surgery, general surgery, or neurosurgery, is prioritized, except in the case of vascular injury. Therefore, orthopedic problems are usually low in surgical priority. Accordingly, it is difficult to perform orthopedic surgery at the appropriate time, and surgery is often delayed. Furthermore, ST patients have difficulties in managing soft tissue damage or swelling, and rehabilitation may not be performed or delayed due to unconsciousness or damage to other areas, which in turn affects functional outcomes after surgery.
This study has the following limitations. First, the sample size was small. Second, the study included only patients who visited the emergency center after trauma. In our hospital where the study was conducted, DRF patients are not allowed to visit through the outpatient hospital unless a medical problem or trauma to the other body areas is observed. Therefore, the number of patients with ML trauma to whom ambulatory care can be easily provided would be relatively lower. Third, the ST group had an ISS of ≥16, but this did not mean that whether their high-energy trauma had directly affected the fracture could be distinguished.
DRFs accompanying high-energy trauma were observed more frequently in younger age patients and male than DRFs accompanying simple trauma. We found that fracture severity and radiological indices after surgery based on the AO/OTA classification were not different between patients who visited the emergency center with high-energy. Furthermore, patients with high-energy DRFs showed worse functional outcomes after surgery and required extra care considering the type of fractures, damages to soft tissues, and condition of the patient’s whole body as well so that they could receive appropriate postoperative management and rehabilitation after fracture treatment.
Acknowledgements
This work was supported by a clinical research grant from Pusan National University Hospital in 2020.
Fig. 1.
Enrollment of patients with distal radius fractures. ML, low-energy monotrauma; MH, high-energy monotrauma; ST, severe trauma.
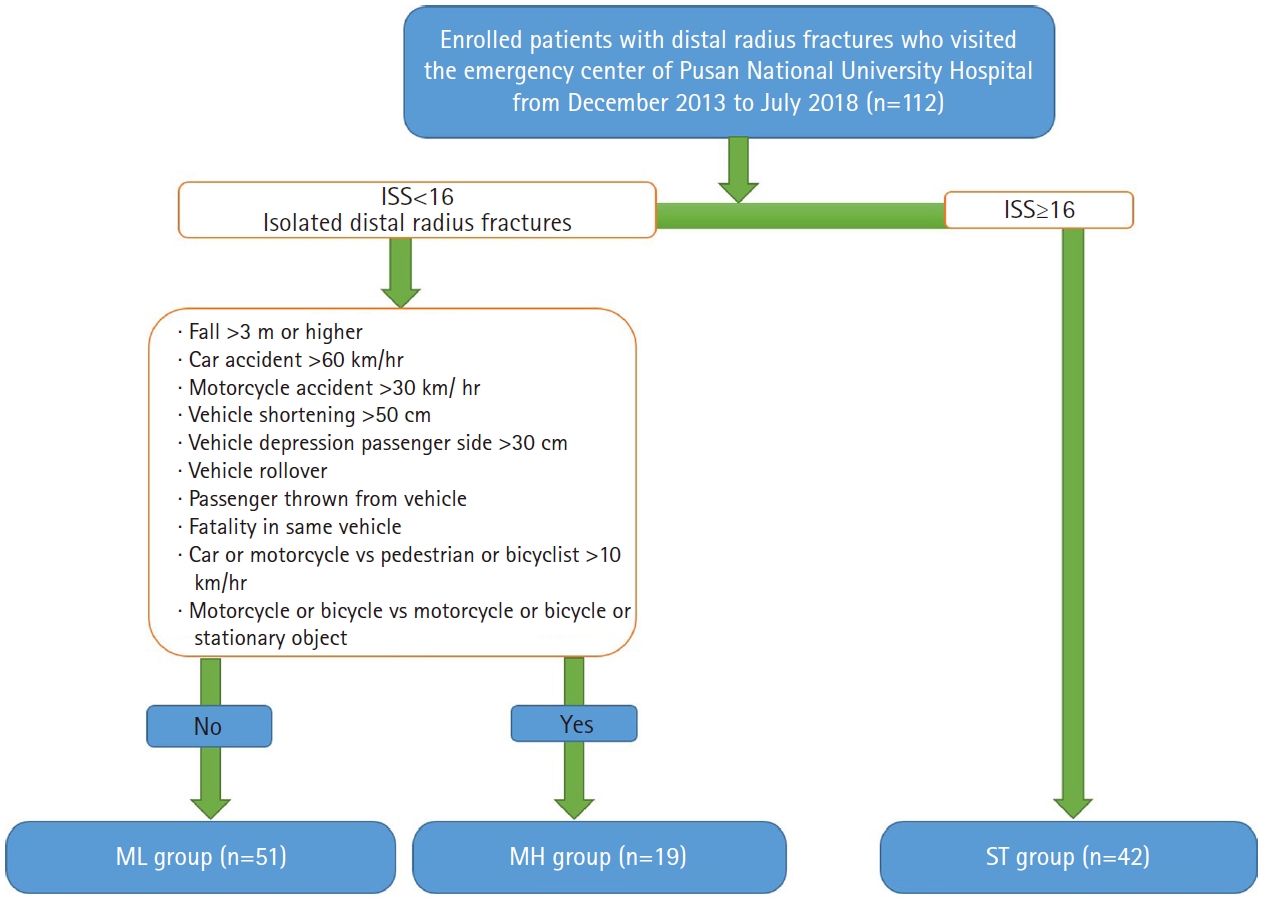
Fig. 2.
Distribution of patients in the three groups according to the AO/OTA classification. (A) Low-energy monotrauma group (n=51). (B) High-energy monotrauma group (n=19). (C) Severe trauma group (n=42). TA, traffic accident.
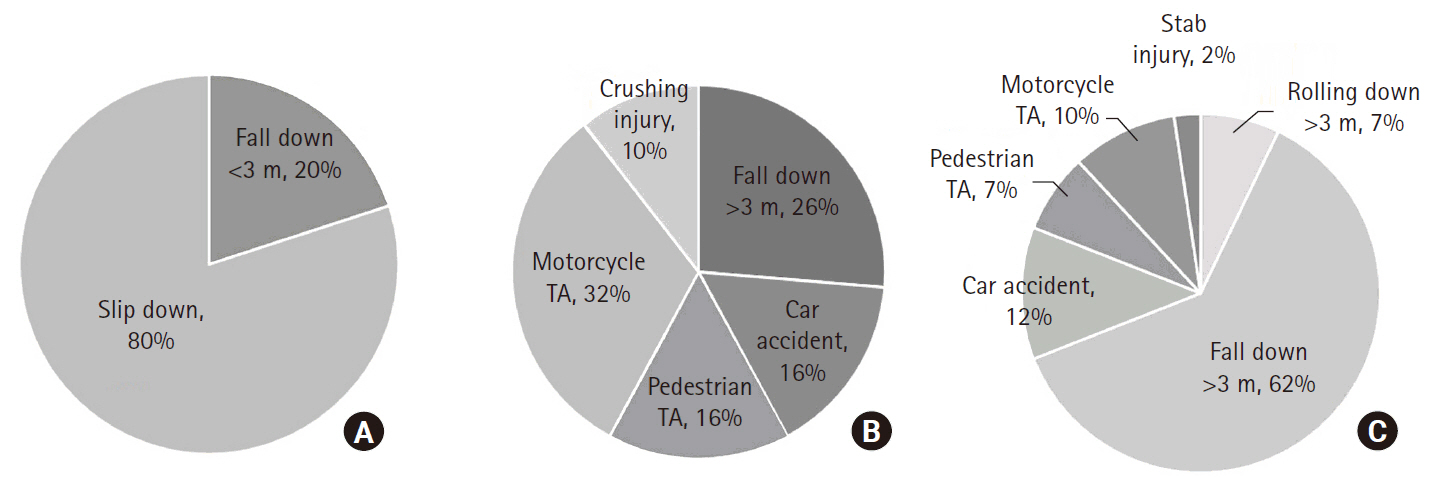
Table 1.
Injury Severity Score
Table 2.
Comparison of sex, age, ISS, AO/OTA classification, ipsilateral injury, and surgical methods among the study groups
Table 3.
Results of the post-hoc test for evaluating significant differences among the study groups
Table 4.
Statistical analysis results of radiological indices and functional outcomes
REFERENCES
1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908-15.


2. MacIntyre NJ, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29:136-45.


3. Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH. Distal radius fractures in older women: a 10-year follow-up study of descriptive characteristics and risk factors. The study of osteoporotic fractures. J Am Geriatr Soc. 2002;50:97-103.


4. Hodel S, Schraner C, Oehme F, et al. Factors predicting adverse outcome in complete intra-articular distal radius fractures. Eur J Trauma Emerg Surg. 2019 Feb 28 [Epub]. https://dx.doi.org/10.1007/s00068-019-01102-8.


5. Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187-96.


6. Ferree S, van der Vliet QM, Nawijn F, et al. Epidemiology of distal radius fractures in polytrauma patients and the influence of high traumatic energy transfer. Injury. 2018;49:630-5.


7. Wæver D, Madsen ML, Rölfing JHD, et al. Distal radius fractures are difficult to classify. Injury. 2018;49 Suppl 1:S29-32.


8. Ferree S, van der Vliet QM, van Heijl M, Houwert RM, Leenen LP, Hietbrink F. Fractures and dislocations of the hand in polytrauma patients: Incidence, injury pattern and functional outcome. Injury. 2017;48:930-5.


-
METRICS

-
- 0 Crossref
- 3,664 View
- 70 Download
- Related articles in Arch Hand Microsurg
-
Prognostic Factors Affected to Distal Radius Fracture in Elderly Patients2003 December;8(4)
Treatment of the Distal Radius Fractures in the Elderly Patients2013 June;18(2)