|
 |
- Search
| Arch Hand Microsurg > Volume 29(1); 2024 > Article |
|
Abstract
This report presents the case of a 23-year-old man with bilateral distal one-third radial shaft fractures and associated distal radioulnar joint disruption, known as Galeazzi fractures, resulting from a fall from a kickboard. After open reduction and plate internal fixation for both radial shafts, the radioulnar joints remained unstable on both sides. We performed arthroscopic repair of the triangular fibrocartilage complex on the left side and used a short arm splint to immobilize the right side. At the 6-month postoperative follow-up, the patient reported mild stiffness in the left wrist, although both sides showed a full range of motion and distal radioulnar joint stability. In conclusion, when achieving anatomic reduction and stable fixation of the radial shaft in a Galeazzi fracture, favorable results can be achieved without additional surgical treatment, even if the distal radioulnar joint is unstable during surgery.
Galeazzi fractures entail fractures of the distal radial shaft along with dislocation of the distal radioulnar joint (DRUJ) [1]. Typically, Galeazzi fractures result from forceful axial loading of the forearm with the wrist extended. They are often referred to as “fractures of necessity” because Galeazzi fracture-dislocations are unstable injuries that necessitate surgical intervention for optimal treatment in adults [2].
Treatment in adults uniformly involves anatomic and rigid fixation of the radius and stabilization of DRUJ [3]. Open reduction and internal fixation (ORIF) for radial shaft fractures is considered the gold standard of treatment [3]. However, there was little agreement concerning the treatment of the DRUJ, mainly stabilized by triangular fibrocartilage complex (TFCC) [3,4]. Various techniques exist for managing the DRUJ problem after radius fixation, including immobilization alone [3,5], transfixing Kirschner wires, ulnar styloid fixation [4,6], and TFCC repair [7]. Finally, the optimal treatment approach remains debated and tends to be considerably chosen by the surgeon’s knowledge and experience [1,8].
In this report, we present the treatment outcomes of a 23-year-old male patient with simultaneous bilateral Galeazzi fracture-dislocation who underwent bilateral ORIF for radius, followed by TFCC repair on the left side and short arm immobilization alone on the right side. We aim to present clinical outcomes related to distinct DRUJ management approaches in cases of bilateral Galeazzi fractures with identical features.
A 23-year-old male, riding a kickboard at 15 km/hour, fell forward and visited the emergency room. He complained of identical forearm and wrist pain, with bilateral distal ulnar head protrusion dorsally. No neurovascular deficit was present on both sides and there were no findings suggestive of generalized laxity such as elbow hyperextension. Initial radiographs showed bilateral radial shaft fracture. Both radial shaft fractures were simple (OTA 22-A2.3), at the same level (70 mm from right wrist joint, 72 mm from left wrist), without severe comminution. The ulnar head was dorsally dislocated, so a bilateral Galeazzi fracture was diagnosed (Fig. 1). Computed tomography imaging findings showed that the sigmoid notch of DRUJ had a ski slope type. Both forearms were temporarily splinted, and the patient underwent surgery 2 days after the injury.
Under general anesthesia, bilateral radial shaft fractures were treated with ORIF using 3.5 mm locking compression plates (Synthes, Oberdorf, Switzerland). At that point, fluoroscopy confirmed an anatomical reduction of the fractured radius shaft and restoration of the DRUJ. During the intraoperative stress test, the ballottement test for the DRUJ revealed easy dorsal dislocation, indicating bilateral DRUJ instability despite achieving anatomic reduction and fixation of the radius shaft (Fig. 2). Since a long arm cast was required to limit pronation supination for healing after TFCC repair, there was concern that both TFCC repairs would interfere with the patient’s daily life. With the patient’s and mother’s consent, it was decided in the first surgery to repair the torn TFCC on the left wrist and maintain the short arm splint on the right wrist as the dominant hand to enable daily activities.
During the arthroscopic examination of the left wrist, a peripheral capsular tear and a positive hook test indicating a proximal component tear were observed. We used the trans-osseous single tunnel technique to repair the TFCC capsular and proximal components, resulting in a stable wrist after the repair (Fig. 3). A long arm supination splint was applied after repair. We performed short arm immobilization alone for the right side without further DRUJ stabilization procedures.
After 2 weeks, the skin sutures on both wrists were removed. The right wrist was placed in a short arm brace for an additional 4 weeks to allow for daily activities, while the left wrist was immobilized in a long arm supination cast for an additional 4 weeks. Six weeks after surgery, all immobilization was discontinued, and range of motion (ROM) was allowed.
Both bilateral radial fractures achieved bone union approximately 10 weeks after surgery (Fig. 4). By this point, wrist joint motion had already recovered to about 80° of palmar flexion and 90° of dorsal flexion on both sides (Fig. 5). According to the ballottement test, there was no DRUJ subluxation in the right wrist, although it was looser than the repaired left side.
At 6-month follow-up, he was free of pain and had a full ROM bilaterally, but appealed subjective stiffness on the left wrist compared to the right side. At his final follow-up, 1 year after surgery, the subjective stiffness on the left side had resolved, with the Disabilities of the Arm, Shoulder, and Hand (DASH) scores of 3.4 for the right wrist and 5.8 for the left wrist (Fig. 6).
The patient consented to have his case published in the case report including all clinical images.
We reported an extremely rare case of bilateral Galeazzi fractures with the same pattern in a young and active 23-year-old man. Following the anatomical reduction and plate fixation of the distal radial shaft fracture, instability was observed in both DRUJs. However, distinct treatments were administered: the left wrist underwent TFCC repair and 6 weeks of long arm supination immobilization, while the right wrist received an utterly opposite approach with 6 weeks of short arm immobilization, allowing DRUJ motion. Nevertheless, both wrists presented similar good clinical and radiologic outcomes.
Galeazzi fractures are relatively rare, representing less than 7% of adult forearm fractures [8]. Bilateral Galeazzi fracture-dislocations in adults are extremely rare, and only six case reports have been described so far (Table 1) [3-5,7,9,10]. Including our case, all previously published cases were male patients in their 20s and 30s who had high-energy injuries. Additionally, for radius, open anatomic reduction and plate fixation were first attempted. Still, DRUJ, it varied from postoperative splint management without additional operative procedures to open reduction and TFCC repair. Despite these differences, clinical outcomes for all cases were reported as favorable.
In our case, our patient had identical injured patterns, including radius shaft fracture level, a length of shortening of radius, a dorsally dislocated ulnar head, a presence and a shape of ulnar styloid fracture, ulnar variance, the shape of sigmoid notch of DRUJ (ski slope shape), and widening of DRUJ. In both wrists, instability in DRUJ also persisted even after anatomic reduction and plate fixation of the radius distal shaft.
The reason for employing different DRUJ managements for each wrist stemmed from considering how postsurgery restrictions would impact the patient’s daily life. If the patient has long arm splint immobilization on both sides, the patient cannot bring hands to his face and daily activities are extremely limited. Additionally, the patient expressed a strong desire to maintain the use of at least one wrist before the operation, even if it necessitated further operation such as TFCC repair to treat clinically significant instability in the future. Therefore, we employed only short arm splint immobilization in the dominant right wrist. On the contrary, a more proactive approach was adopted for the left wrist, entailing arthroscopic TFCC repair, and the utilization of supination restriction splints and casting for a duration of 6 weeks.
Consequently, although mild laxity was noted in the right wrist, mild stiffness was reported in the left wrist 6 months after surgery. Remarkably, both wrists exhibited equally positive outcomes at the 1-year follow-up.
Rettig and Raskin [11] classified these fractures into two types based on the location of the fracture from the midarticular surface of the distal radius. Type I fractures occurred within 7.5 cm from the midarticular surface of the distal radius and had a higher incidence of DRUJ instability requiring operative fixation (55%, 12 patients). Our case belonged to type 1 fracture and both wrists identically presented an unstable but reducible DRUJ.
Most of the previous literature recommends long arm immobilization for 3 to 6 weeks for the rehabilitation of Galeazzi fracture [8], and only a few literature support short arm immobilization. Gwinn et al. [12] reported good results by performing early motion in the stable Galeazzi fractures. However, comparative studies on the role of short arm immobilization after internal fixation of radius in Galeazzi fractures could not be confirmed. The reason why no further dislocation occurred in the right hand is presumed to be as follows. For the first, a short arm immobilization still can reduce DRUJ movement to some extent [13,14]. Second, surrounding dynamic stabilizers such as the flexor carpi ulnaris and extensor carpi ulnaris contribute to the stability of the DRUJ after anesthesia [15]. This suggests that the intraoperative stress test could not accurately reflect DRUJ instability.
There are limitations in making conclusions based on a single case, but even in unstable DRUJ, immediate ROM did not cause chronic instability, and recovery was faster than in the opposite wrist where TFCC was repaired. The implications of our case are as follows. A short arm immobilization is considerable for unstable Galeazzi fractures after rigid fixation of the radius. The stress test performed intraoperatively could have a poor correlation with DRUJ stability after anesthesia.
If wrist pronation and supination are allowed immediately, DRUJ instability may remain and secondary surgery for TFCC repair may be performed at a later date. There is also no evidence that delayed TFCC repair reduces functional outcomes or increases the incidence of complications such as osteoarthritis.
When achieving anatomic reduction and stable fixation of the radial shaft in a Galeazzi fracture, favorable results can be achieved without additional surgical treatment, even if the DRUJ is unstable during surgery.
Fig. 1.
Preoperative anteroposterior (A) and lateral (B) radiographs of the right wrists demonstrating a Galeazzi fracture-dislocation. On the left side, an almost identical injury pattern was present (C, D). Both radial fractures were located 9 to 10 cm proximal from the joint, and the ulnar head was dislocated dorsally.
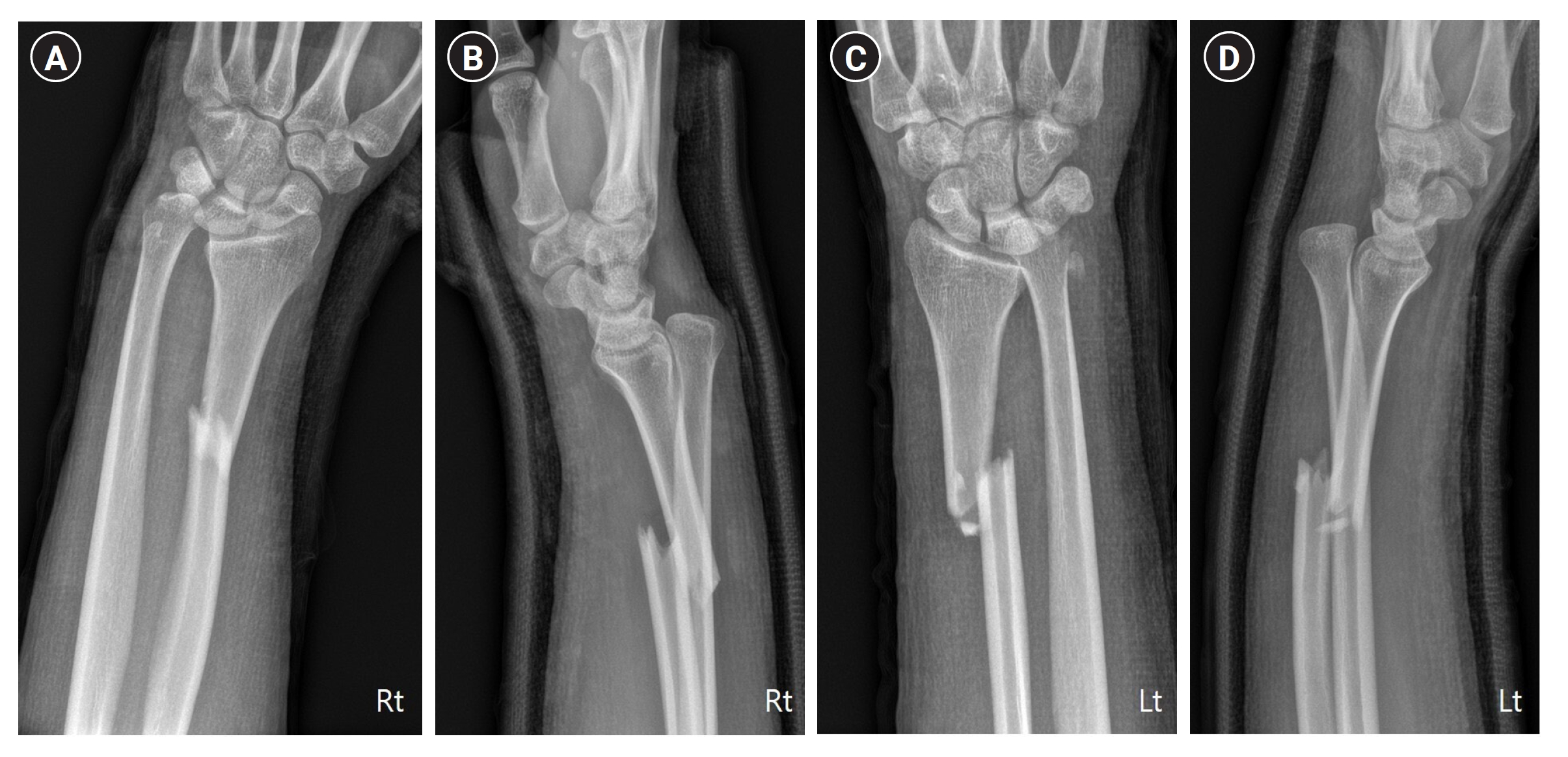
Fig. 2.
After fixation of the radius fractures, intraoperative stress tests were performed (A, B). Dorsal subluxation of the ulnar head was found in the full pronation position (A).

Fig. 3.
On the left side, we performed arthroscopic triangular fibrocartilage complex repair using a bone tunnel. Torn triangular fibrocartilage complex was found (A). We made a bone tunnel (B) and repaired the triangular fibrocartilage complex (C, D).
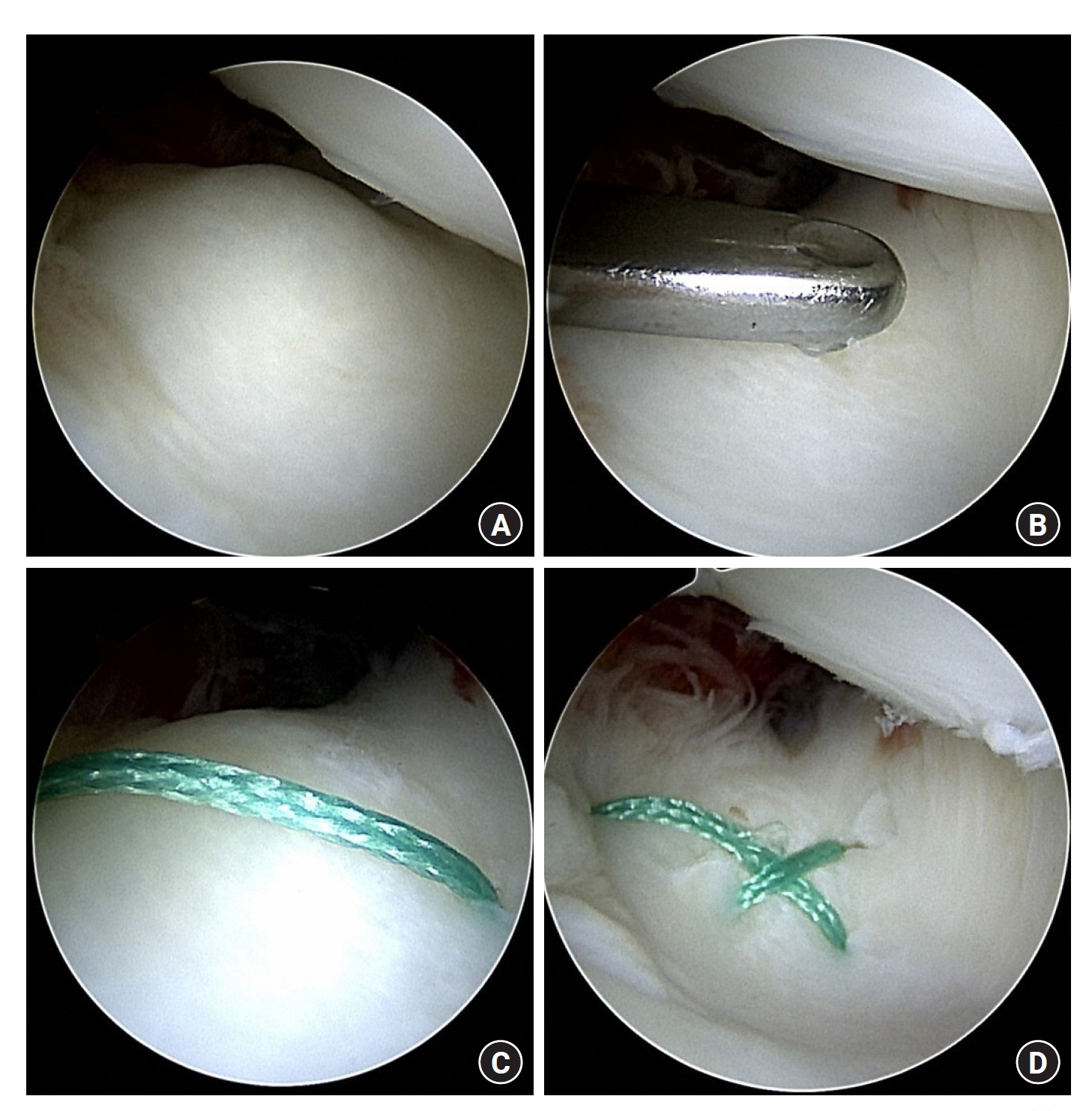
Fig. 4.
At a 10-week postoperative follow-up visit, plain anteroposterior (A, C) and lateral (B, D) radiographs presented sound union without distal radioulnar instability.
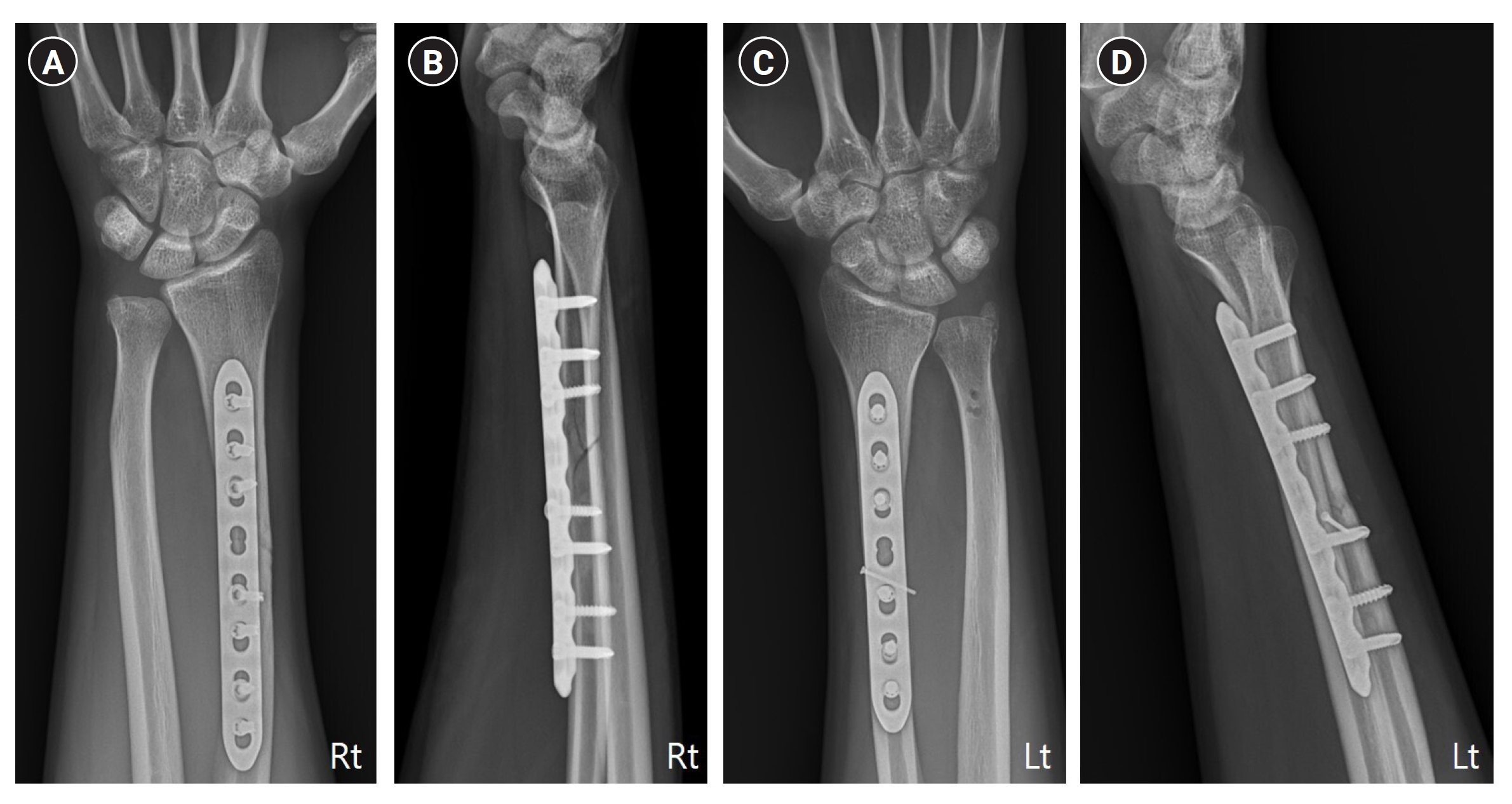
Fig. 6.
Plain radiographs at a 1-year postoperative follow-up visit show bony union with a reduced distal radioulnar joint. Anteroposterior and lateral views of the right (A, B) and the left (C, D) wrists were shown.
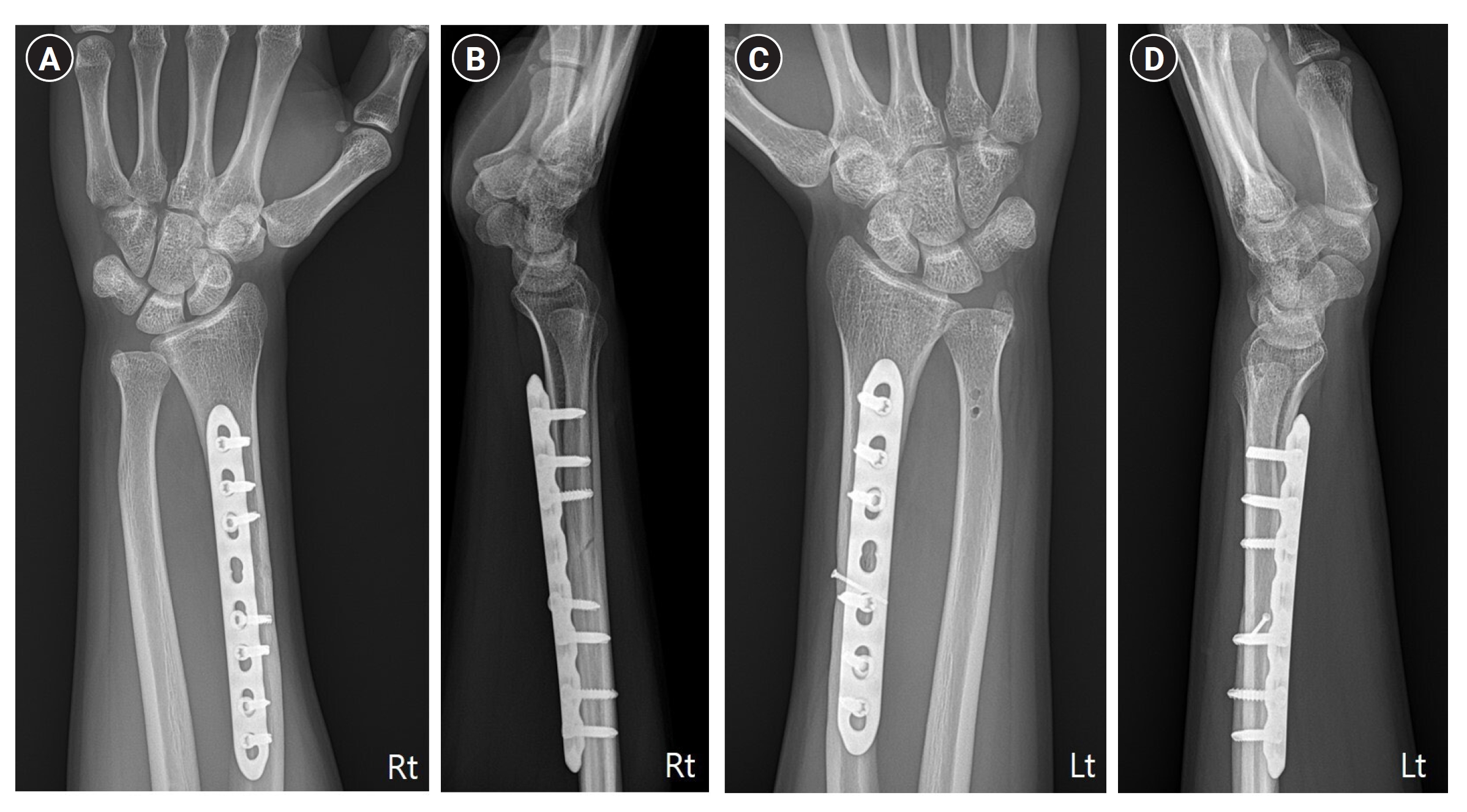
Table 1.
Summary of previously reported bilateral Galeazzi’s fracture case
| Study (year) | Sex/age (yr) | Injured mechanism | Injured arm |
Operation |
Postoperative immobilization | ROM start | Outcome | |
|---|---|---|---|---|---|---|---|---|
| Radius | DRUJ management | |||||||
| Sivakumaran et al. [3] (2021) | Male/24 | Motorbike accident | Right | OR 6 holes DCP | None | Bilateral above-elbow back slab | 3 wk | 10-wk union with full ROM |
| Left | OR 7 holes DCP | |||||||
| Panagopoulos et al. [5] (2021) | Male/31 | Bicycle accident with a car | Right | OR 3.5-mm 8 holes LCP | None | Long forearm cast | 4 wk | 6-yr follow-up, full ROM without pain. |
| Left | OR 3.5-mm 8 holes LCP | Mayo wrist score 95 | ||||||
| Chatterjee [7] (2014) | Male/36 | Fall from horse | Right | OR 7 holes LC-DCP | Open TFCC repair with collateral ligament repair followed by transfixing K-wire | Custom-made above-elbow braces with hinge at elbow and wrist immobilized in 30° supination | 4 wk after K-wire removal | Painless, stable, and functional wrists at 4 mo |
| Left | OR 7 holes DCP | None | ||||||
| Komura et al. [9] (2012) | Male/24 | Motorcycle accident | Right (1st operation) | OR 3.5-mm 7 holes LC-DCP | None | Supination splint | Immediately | Full ROM with mild pain and Discomfort at final follow-up |
| Right (2nd operation) | None | Tension band wiring | ||||||
| Left (1st operation) | External fixator | None | Full ROM with mild laxity but without pain at final follow-up | |||||
| Left (2nd operation) | 2.4-mm long distal radius bridging plate with bone graft | None | ||||||
| Nanno et al. [4] (2011) | Male/32 | Motorbike accident | Right | OR 3.5-mm DCP | Tension band wiring | Long arm splint | 4 wk | 0–135 elbow flexion, 60/60 wrist dorsi/volar flexion, full supination at 6-yr follow-up |
| Left | ||||||||
| Borens et al. [10] (2006) | Male/25 | Motorcycle accident | Right | OR 3.5-mm DCP | None | Symmetric pain-free almost ROM at 20 mo after injury | ||
| Left | OR 3.5-mm DCP | Open reduction, capsule, ECU tendon sheath repair, K-wire | Bilateral supination splint | 6 wk | ||||
| Left (2nd operation) | None | Darrach procedure | ||||||
References
1. Sebastin SJ, Chung KC. A historical report on Riccardo Galeazzi and the management of Galeazzi fractures. J Hand Surg Am. 2010;35:1870-7.



3. Sivakumaran D, Pathinathan K, Madushanger SR, Gunawardena PM, Dimantha WH, Munidasa D. Bilateral symmetrical pronation type of Galeazzi fracture following high-speed motor traffic crash: a case report. Int J Surg Case Rep. 2021;85:106284.



4. Nanno M, Sawaizumi T, Takai S. Case of bilateral Galeazzi fractures associated with dislocation of the right elbow. J Nippon Med Sch. 2011;78:384-7.


5. Panagopoulos A, Solou K, Tatani I, Kouzelis A, Kokkalis Z. A case of bilateral Galeazzi fracture-dislocations. Cureus. 2021;13:e17491.



7. Chatterjee D. Early rehabilitation in unstable bilateral Galeazzi fracture dislocation: role of transfixing K wires. Saudi J Sport Med. 2014;14:168-171.

9. Komura S, Nonomura H, Satake T, Yokoi T. Bilateral Galeazzi fracture-dislocations: a case report of early rehabilitation. Strategies Trauma Limb Reconstr. 2012;7:99-104.




10. Borens O, Chehab EL, Roberts MM, Helfet DL, Levine DS. Bilateral Galeazzi fracture-dislocations. Am J Orthop (Belle Mead NJ). 2006;35:369-72.

11. Rettig ME, Raskin KB. Galeazzi fracture-dislocation: a new treatment-oriented classification. J Hand Surg Am. 2001;26:228-35.


12. Gwinn DE, O'Toole RV, Eglseder WA. Early motion protocol for select Galeazzi fractures after radial shaft fixation. J Surg Orthop Adv. 2010;19:104-8.

13. Kim JK, Kook SH, Kim YK. Comparison of forearm rotation allowed by different types of upper extremity immobilization. J Bone Joint Surg Am. 2012;94:455-60.


-
METRICS

-
- 0 Crossref
- 1,277 View
- 11 Download
- Related articles in Arch Hand Microsurg
-
Arthroscopic Repair of Triangular Fibrocartilage Complex Tear2020 September;25(3)
The Role of Arthroscopy in Management of Distal Radius Fractures2001 December;6(2)
Open Repair of Triangular Fibrocartilage Complex Type 1B Tear2014 June;19(2)
Ganglion of the Triangular Fibrocartilage Complex: A Case Report2011 March;16(1)