|
 |
- Search
| Arch Hand Microsurg > Volume 27(1); 2022 > Article |
|
Abstract
An injury of a peripheral nerve may require reconstruction for motor and sensory function recovery. However, if the nerve defect is long, especially in the lower extremities, reconstruction with successful functional recovery has proven to be difficult. We documented a case of bilateral vascularized sural nerve graft repair of a large and long sciatic nerve defect following malignant tumor resection on the posterior thigh. Although we were unable to achieve satisfactory outcomes in motor function recovery, we did achieve some degree of sensory function recovery.
Peripheral nerve injury needs repair in order to restore motor and sensory function. When direct end-to-end repair is not possible, an autologous nerve graft is usually used for reconstruction of the nerve defect [1]. Compared with the reconstruction of upper extremity nerve, the sciatic nerve has a larger cross-sectional area which makes it difficult for reconstructive surgeons to obtain positive outcomes with nerve grafts in motor and sensory function recovery when reconstructing the sciatic nerve. Many studies demonstrated the efficacy of the vascularized nerve graft especially in poor vascularized beds and long defects [2,3]. In this report, we used a bilateral vascularized sural nerve graft for reconstruction of an 8 cm in length sciatic nerve defect with poor vascularized bed after tumor resection. Although we could not get satisfactory results in the motor function recovery, we did acquire some protective sensation in the sole of foot which we focused on preoperatively.
A 63-year-old male patient with a history of diabetes mellitus and chronic kidney disease visited a local clinic with complaints of a palpable mass of left posterior thigh, numbness of left sole, and tingling sensation of left popliteal fossa, which first appeared three years earlier. Excisional biopsy revealed Ewing’s sarcoma with a positive surgical margin. The patient was referred to our hospital for further evaluation and management. Magnetic resonance imaging examination revealed a 1.0×6.0×2.0-cm sized remaining mass in the left posterior thigh. The mass was located in front of hamstring muscle and attached to the sciatic nerve (Fig. 1). And simultaneous tumor resection followed by nerve reconstruction was planned. Intraoperatively, the tumor mass was shown adhered to the sciatic nerve and involved surrounding muscles (Fig. 2). Wide resection including semitendinosus, semimembranosus, adductor Magnus muscle, and adjacent sciatic nerve was performed. After resection of the mass, 8-cm sized sciatic nerve defect was found around 4 cm above a popliteal fossa (Fig. 3).
For reconstruction of the sciatic nerve defect, we used a bilateral vascularized sural nerve graft because the length of the defect was 8 cm with large cross-sectional area and poor vascularized bed. We harvested sural nerves together with lesser saphenous vein and fascia from both lower legs and it provided 50 cm of graft material (Fig. 4).
As the sural nerve has much smaller cross-sectional area and the percentage of the tissue that contains valuable neural structures, represented as the fascicles compared with the sciatic nerve, harvested 50 cm graft material is insufficient to reconstruct the 8-cm defect of sciatic nerve properly. Instead of harvesting additional nerve, we focused the repair on the tibial division mainly not on the peroneal division from desire to restore sensory function. So, eight fascicular segments were applied to the tibial division and four to the peroneal division. A fibrin glue was used to seal the suture sites. Vascular anastomosis was made at three sites: (i) between two lesser saphenous veins, (ii) between the lesser saphenous vein and alongside artery, and (iii) between the lesser saphenous vein and alongside vein (Fig. 5). After reconstruction of the nerve defect and vascular anastomosis, both donor site and left posterior thigh were closed primarily. The final diagnosis was a malignant peripheral nerve sheath tumor.
After surgery the patient was maintained in prone position with mild knee extension for prevention of vascular compression and nerve stretching for 5 days. And hand-held Doppler was used to confirm the flow of anastomosis site. From 1 week after surgery, the patient was encouraged to ambulate using walker. There were no wound complications including seroma, infection and dehiscence during admission, and the patients was discharged on postoperative day 15.
We followed up with the patient for 20 months postoperatively to check function restoration, local recurrence and distal metastasis. There was no motor or sensory recovery until 2 months following surgery. However, Tinel sign was positive 4 months after surgery, with minimal protective sensation in the popliteal fossa region. The patient felt some improvement in the sole of the foot 18 months after surgery but was unable to walk without the assistance of a cane. Electrophysiological examination of lower extremities was performed twice; 3 month and 15 month after surgery. In the motor nerve conduction study of the sciatic nerve, the H-reflex test and the F-wave test were all absent in the left lower extremity, and there was no difference between two tests. (Compound muscle action potential for the sciatic nerve were stimulated in the gluteal fold, recorded in the gastrocnemius and tibialis anterior, respectively, and were not evoked). However, in the medial and lateral plantar sensory study, which is the sensory component of the tibial nerve (part of sciatic nerve), it was not evoked at 3 month postoperatively, but it was evoked at 15 months postoperatively. Although the latency and amplitude were abnormal compared to the unaffected side.
Although we could not get satisfactory results in motor recovery, minimal sensory recovery was achieved. And evaluation of local recurrence and distal metastasis shows there are no recurrence and metastasis at 20 months postsurgery in image study (Fig. 6).
Written informed consent was obtained for publication of this case report and accompanying images.
The sciatic nerve is the longest and widest peripheral nerve of a human body. It provides motor innervation to the posterior thigh muscles and all muscles of the leg and foot. It also provides sensory innervation of the skin of the foot and lower leg except for the medial thigh which is innervated by the saphenous nerve [4].
Although sciatic nerve injury is considerably less common than upper extremity injury, it can be caused by iatrogenic injury (injection, hip surgery), trauma, and mass excision.
Despite the advancement of microsurgical repair methods, functional recovery following peripheral nerve restoration remains poor. However, a sciatic nerve damage can have a serious influence on the life of a patient. As previously stated, it can result in both motor and sensory function abnormalities. Loss of sensation in the foot, in particular, might result in a pressure sore and infection, which can lead to limb amputation.
Direct end-to-end epineural suture is the gold standard if tension-free nerve repair is feasible. When there is too much strain for direct end-to-end repair, nerve grafts or conduits are generally considered. Numerous conduits have been reported; however, their use is limited in specific case like with short nerve defect. So, when it comes to long nerve defects that cannot be repaired by direct suture or using a nerve conduit, autogenous nerve grafts are the only suitable options for reconstruction [1]. The sural nerve is a common candidate for grafting and has been studied extensively in long nerve defect.
The nerve graft can be done by conventional method or with vascularization. The free vascularized nerve graft was first reported by Taylor and Ham [2] in 1976 and many studies have been performed and demonstrated the efficacy of vascularized nerve graft especially in the upper extremity. In 1992, Doi et al. [5] used 27 vascularized and 22 conventional sural nerve grafts in upper extremity nerve reconstructions. Compared with conventional nerve graft, vascularized nerve graft shown has superior outcomes in terms of the rate of axonal regeneration, rate of electromyography returns, and restoration of motor and sensory functions. In 1988, Mackinnon et al. [6] showed superior sensory recovery in vascularized radial nerve graft than conventional sural nerve graft in reconstruction of median nerve defect. Many other published reports showed better outcomes in vascularized nerve grafts compared to conventional nerve grafts under certain clinical conditions by providing faster and better regeneration. Of course when nonvascularized nerve graft working well, the vascularized nerve grafts are not considered due to additional complexity, time consuming and donor site morbidity. So D’Arpa et al. [7] suggested the indication of vascularized nerve graft in the following scenarios; (1) nerve gaps longer than 6 cm, (2) nonvascularized beds, (3) composite defects requiring a free flap, (4) proximal lesions, (5) long denervation times, (6) planned radiation therapy, (7) pedicled vascularized nerve graft in the same field, and (8) advanced age.
However, it can be challenging to use for patients with long sciatic nerve defect because of the larger cross-sectional area compared with the nerve of upper extremity and face. The rates of success in research on the reconstruction of long sciatic nerve defects with nerve grafts depend on a number of factors, including the length and location of the defect, the implicated branch (peroneal or tibial division), the length of time until surgery, age, and comorbidities. And poor outcomes are mainly associated with peroneal division, delayed surgery (delay of >4 months), and long defect (length of >5 cm) [8].
In our cases, there was an 8-cm sized sciatic nerve defect which involved both peroneal and tibial division with poor vascularized bed because many surrounding tissues including muscle were resected en bloc. Well-vascularized bed is essential for successful transfer of the conventional nerve grafts. And as mentioned above, indications for vascularized nerve grafts included the nonvascularized bed and longer than 6-cm nerve gaps. So we decided to use the vascularized sural nerve graft from both lower legs, with the primary goal of restoring plantar sensation which was innervated by the tibial division during sciatic nerve repair. Because bilaterally harvest graft material is not sufficient to reconstruct both division and sensory loss in these areas can lead to complications like ulceration. Unfortunately, the patient exhibited no motor recovery. But more long-term follow-up is needed as Gaul [9] in 1982 noted that the intrinsic muscle could continue to improve for 5 years or more in ulnar nerve and Nicholson and Seddon [10] in 1957 reported sensory function improving from 38% at 3 years to 65% at 5 years in median nerve.
Despite some persisting perceptual deficit, we were able to produce the intended reduced protective sensation in the sole of the foot that we had planned for.
The limitations of our study are that the follow-up period is relatively short with one case and the evidence accumulated is not decisively in favor of vascularized nerve grafts although there may be indications. We also regret not doing more prolonged and careful protection which recommended 12 weeks for nerve repair, with early ambulation and discharge. And as the sensory nerve action potential test means the continuity of nerve, it is not sufficient for evaluating the restoration of perception. More reliable test like two-point discrimination test, Semmes-Weinstein monofilament test, or other sensory perception tests including sensory mapping, vibratory perception thresholds, and current perception thresholds.
Given the aforementioned, a bilateral vascularized sural nerve transplant may be a viable alternative for the repair of lengthy sciatic nerve deficits in order to avoid complications that might lead to limb amputation.
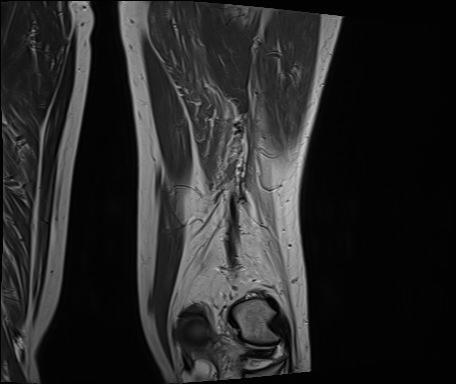
Fig. 1.
Magnetic resonance images of the left posterior thigh. (A) Sagittal view. (B) Axial view. In front of the hamstring muscle, a mass measuring about 1.0×6.0×2.0 cm attached to the sciatic nerve is shown.
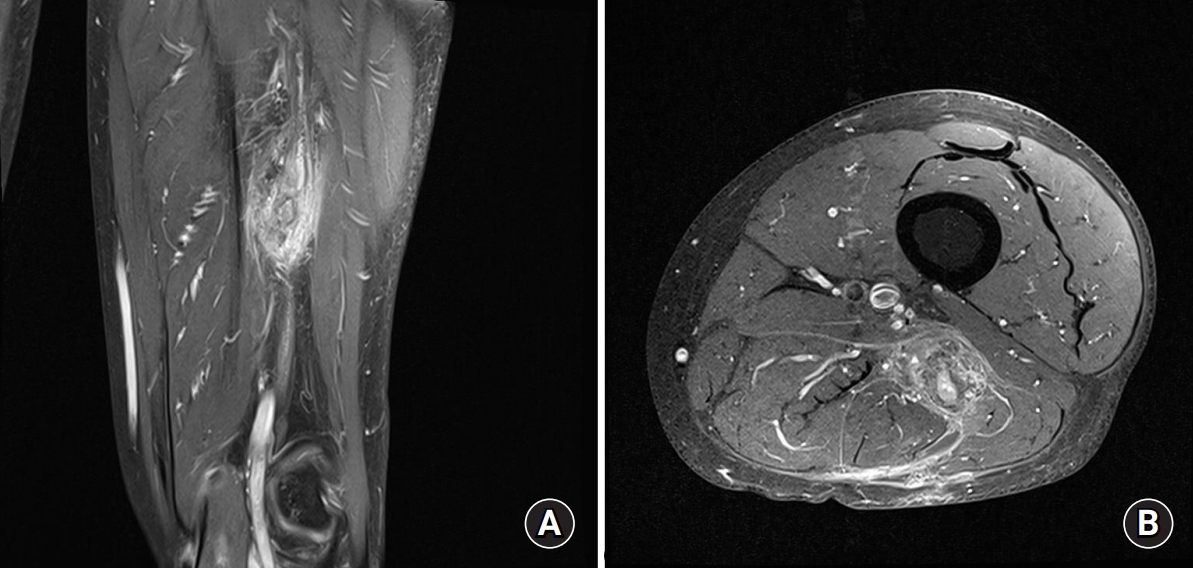
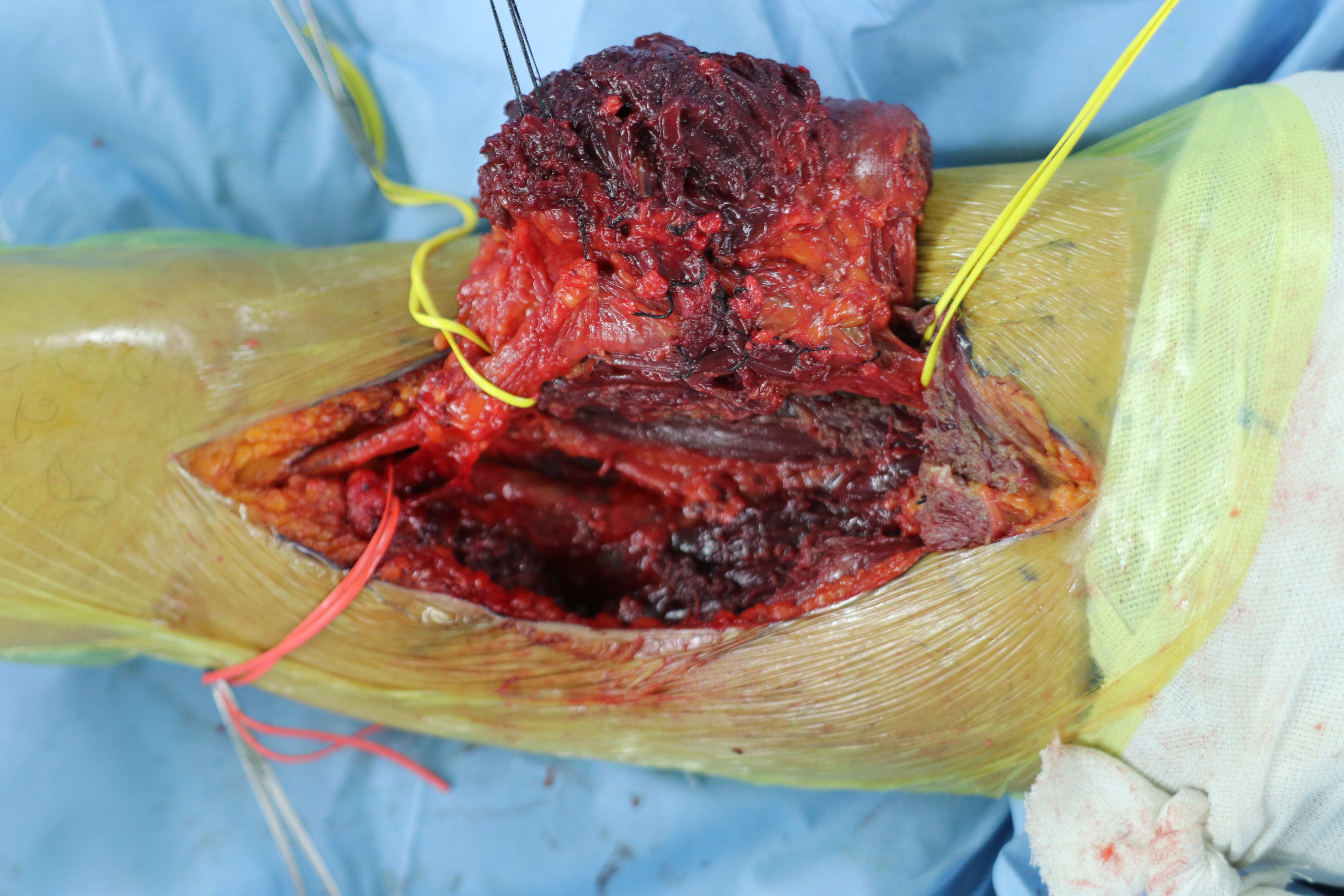
Fig. 3.
After wide excision of the tumor mass including the sciatic nerve and surrounding tissues, an 8-cm sciatic nerve defect is shown around 4 cm above the bifurcation site.
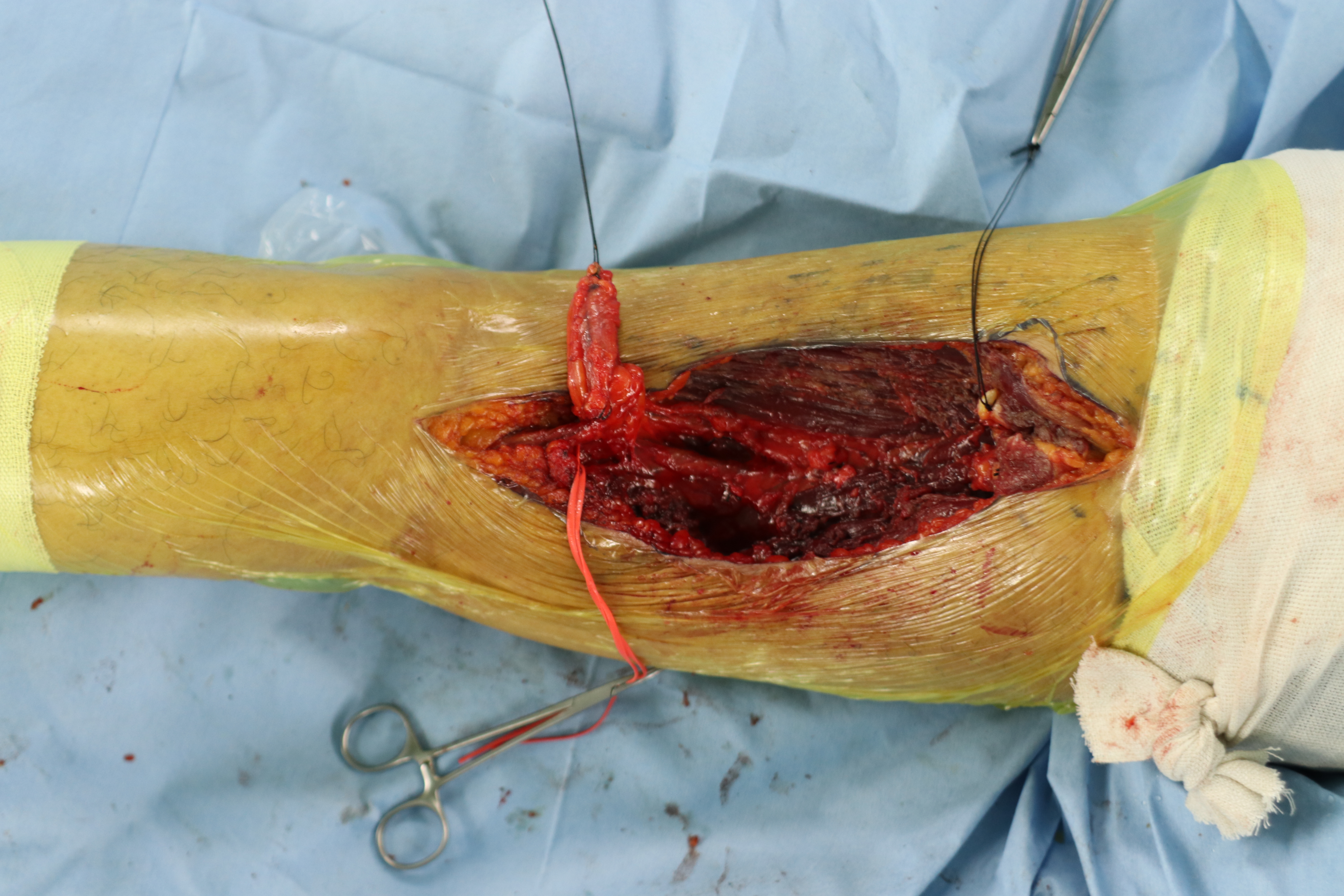
Fig. 4.
The sural nerve, including the lesser saphenous vein and the fascia, was elevated and harvested en bloc to form a vascularized flap from both lower legs. (A) Right lower leg. (B) Left lower leg. (C) Vascularized sural nerve by the lesser saphenous vein and the fascia.

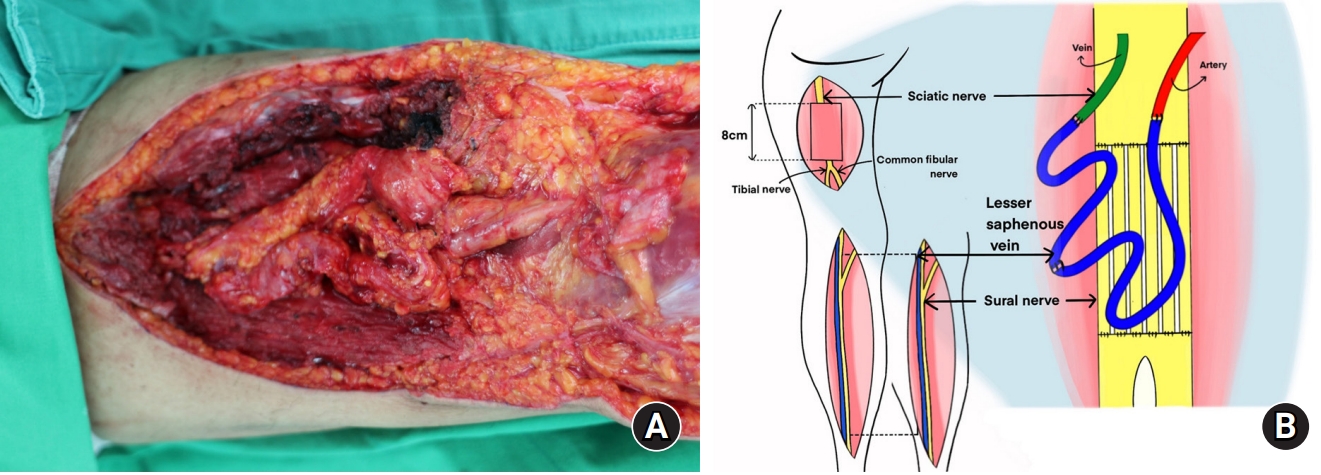
Fig. 5.
Repair of the sciatic nerve with the harvested bilateral vascularized sural nerve and vascular anastomosis at three sites, between two lesser saphenous veins, between the lesser saphenous vein and alongside the artery, and between the lesser saphenous vein and alongside the vein. (A) Intraoperative image. (B) Schematic diagram.
References
1. Grinsell D, Keating CP. Peripheral nerve reconstruction after injury: a review of clinical and experimental therapies. Biomed Res Int. 2014;2014:698256.



2. Taylor GI, Ham FJ. The free vascularized nerve graft. A further experimental and clinical application of microvascular techniques. Plast Reconstr Surg. 1976;57:413-26.

3. Terzis JK, Kostopoulos VK. Vascularized nerve grafts and vascularized fascia for upper extremity nerve reconstruction. Hand (N Y). 2010;5:19-30.


4. Burks SS, Levi DJ, Hayes S, Levi AD. Challenges in sciatic nerve repair: anatomical considerations. J Neurosurg. 2014;121:210-8.

5. Doi K, Tamaru K, Sakai K, Kuwata N, Kurafuji Y, Kawai S. A comparison of vascularized and conventional sural nerve grafts. J Hand Surg Am. 1992;17:670-6.


6. Mackinnon SE, Kelly L, Hunter DA. Comparison of regeneration across a vascularized versus conventional nerve graft: case report. Microsurgery. 1988;9:226-34.


7. D’Arpa S, Claes KE, Stillaert F, Colebunders B, Monstrey S, Blondeel P. Vascularized nerve "grafts": just a graft or a worthwhile procedure? Plast Aesthet Res. 2015;2:183-94.

8. Kline DG, Kim D, Midha R, Harsh C, Tiel R. Management and results of sciatic nerve injuries: a 24-year experience. J Neurosurg. 1998;89:13-23.


-
METRICS

-
- 1 Crossref
- 2,899 View
- 76 Download
- Related articles in Arch Hand Microsurg