|
 |
- Search
| Arch Hand Microsurg > Volume 25(4); 2020 > Article |
|
Abstract
Purpose
Although plate osteosynthesis is commonly used to treat proximal ulna fracture, its treatment method is controversial because of complications such as large incision, long operation time, and soft tissue injury. Therefore, intramedullary headless compression screw (HCS) and Steinmann pin are considered as alternative treatment options. In this study, we aim to compare bending strength of plate and cortical screws, HCS, and Steinmann pin for proximal ulnar shaft fracture with sawbone.
Methods
Transverse type fractures were made intentionally at the distal 7 cm from the proximal end of ulna sawbones and fixated with plate, HCS, and Steinmann pin after reduction. Three-point bending tests were performed with total of 21 sawbones, seven pieces for each group.
Results
Average ultimate bending strength for each group was as follows; 521.7 N for plate fixation group, 706.4 N for HCS fixation group, and 812.6 N for Steinmann pin fixation group. Statistically significant results were observed among the three groups (p<0.01). When two groups were compared separately, Steinmann pin fixation and plate fixation (p<0.01), Steinmann pin and HCS fixation (p=0.047) showed statistical significance. There was a significant trend between HCS and plate fixation group (p=0.064).
Conclusion
HCS and Steinmann pin fixation showed higher bending strength when compared to plate fixation for proximal ulnar shaft fracture in sawbone. Although further studies are needed, HCS and Steinmann pin fixation are promising fixation methods that may be used as an alternative to plate fixation.
Isolated ulna fracture is a type of fracture that commonly occurs in forearm injury [1]. Isolated ulnar shaft fracture looks benign, but its treatment method is controversial because of complications such as nonunion, skin irritation, and loss of motion. Fundamentally, conservative treatment using splint or cast can be performed only for nightstick fractures with low displacement and low angulation [1]. In this case, the union rate is close to 96% or higher, but it takes a longer time to start rehabilitation [2]. Besides this nondisplaced fracture type, most proximal ulnar shaft fractures are unstable that most proximal ulna shaft fractures are recommended for surgery [3,4].
Among operative techniques, plate osteosynthesis is generally preferred because it has high union rate [5-9]. However, fixation with plate requires large incision and periosteal stripping so that it can interfere with blood supply, suppress revascularization, and cause soft tissue injury [10]. It can also bring about nerve palsy, irritation of skin, and it has a high possibility of refracture after implant removal [10]. An alternative treatment to overcome this problem is intramedullary nailing. Intramedullary nailing is a biological method in that it has less stripping of periosteal blood supply, preserves soft tissues including fracture hematoma, and avoids skin irritation [10]. Of course, intramedullary nails have disadvantages of additional incision for interlocking screw and standardized size to be cut for operation [10].
In this study, we are introducing techniques using intramedullary cannulated headless compression screw (HCS) and intramedullary Steinman pin. Among these various techniques, we applied plate, intramedullary HCS, and intramedullary Steinman pin fixation to the sawbones to conduct a comparative study on which method has the strongest bending strength.
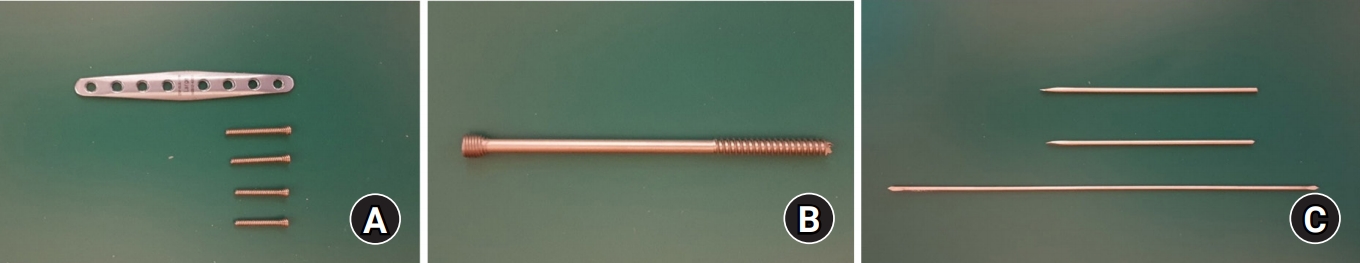
We used ulna sawbones of same size and thickness. Total 21 sawbones (#1017; Sawbones Pacific Research Laboratories, Vashon Island, WA, USA) were used and were separated into three groups by fixation methods, seven pieces for each. Three groups were as follows; group with plate fixation, group with HCS fixation, and group with Steinmann pin fixation. Transverse type fractures (AO/OTA classification, 2U2A3a) were made intentionally with saw at the distal 7 cm from the proximal end of ulna sawbones. Then fractured bones were firmly fixed by every three methods after reduction. We used ulna osteotomy plate (eight holes with 2.5 mm in thickness and 70 mm in length; Jeil Medical, Seoul, Korea), and self-tapping cortical screws (2.8 mm in diameter; Jeil Medical) for plate group (Fig. 1A). Arix headless cannulated compression screw (6.0 mm in diameter and 120 mm in length; Jeil Medical) was used for the HCS group (Fig. 1B), and two Steinmann pins (3.2 mm in diameter and 240 mm in length; Solco Biomedical, Pyeongtaek, Korea) were used for Steinmann pin fixation (Fig. 1C). The plate was placed medial to the bone and symmetric to the fracture line as the center. Two self-tapping cortical screws were fixed on each side. Intramedullary headless cannulated compression screw was inserted from the proximal ulna toward the head with thread crossing the fracture line. Two intramedullary Steinman pin fixations were inserted in the same direction as that of the intramedullary headless cannulated compression screw. The reason for using the pin cut in half is that it can be fit to the diameter only if two are used and also can match the length of HCS. All fractured bones with fixation through each method were tested with three-point bending test system (ElectroPuls E3000; Instron, Norwood, MA, USA) (Fig. 2). Ulnar bone was fixed tightly at 4-cm intervals from fracture line to prevent the rotation force from being generated. Stress was applied vertically from above to fracture site with fixation until displacement was observed (Fig. 3). Next, the amount of applied stress force and displacement values were graphed.
For statistical analysis of comparing average bending strength, Kruskal-Wallis test was applied with the averages and ranges due to lack of sample size. The post-hoc test using the Bonferroni method was used to evaluate significant differences between the groups. The level of p-value was set at 0.05 and SAS ver. 9.4 (SAS Institute, Cary, NC, USA) were used for statistical analysis.
Since it is not a research targeting human or human derivatives, the approval of Institutional Review Board was waived.
Average ultimate bending strengths of proximal ulna shaft fracture for each group were as followed: 521.7 N (range, 339.5 to 675.8 N) for plate and screws fixation group, 706.4 N (range, 662.9 to 725.2 N) for cannulated HCS fixation group, and 812.6 N (range, 794.0 to 832.7 N) for Steinmann pin fixation group (Table 1). With the Kruskal-Wallis test, average bending strength between three groups showed significant differences (p<0.001) (Table 2). Post-hoc test was done to compare each combination of two groups. Significant difference was seen in two combinations; Steinmann pin vs. plate fixation group (p<0.001), and Steinmann pin vs. HCS fixation group (p=0.047). There was a significant trend in one combination; HCS vs. plate fixation group (p=0.064) (Table 3).
Although many surgical methods have been introduced in the ulna shaft fracture, open reduction and internal fixation with plate and screws is widely used for high union rate [5-9]. The axial and rotational alignment can be accurately restored only by correcting the fracture site visually. Direct healing is induced by compressing the fracture site using DCP and cortical screws while maintaining complete reduction [11-13].
However, this plate osteosynthesis also has some disadvantages. Because of the large incision on skin and soft tissue injury due to dissection, it can interfere with blood circulation as the fracture heals [10]. In addition, proximal ulna has almost no soft tissue structure, so when plating is performed, patients may complain of skin irritation after surgery [14]. Another problem is that due to the curved anatomical structure of the ulna, accurate plating may be difficult. Of course, there are anatomical plates manufactured considering such an anatomical structure, pyromellitic dianhydride (PMDA) and oxydianiline (ODA) required for plating. However, it is not technically easy because it does not take into account the individual patient’s anatomical variance, and can lead to malunion or Monteggia fracture dislocation if it goes wrong [15]. The last drawback is that the bone itself is weak due to the bone hole that is drilled during plating, and there is a high possibility of refracture when removing the internal fixation device [1,10].
Intramedullary nail is proposed as a method to replace the plate osteosynthesis. Intramedullary nailing is functional and shows union rate similar to plating, and has high patient satisfaction [16,17]. Unlike the plate osteosynthesis, intramedullary nail is easy for revascularization because it does not undergo periosteal stripping, has a small size of incision and minimal range of soft tissue dissection. This has the advantage of making the callus better and becoming a stronger union [10].
However, intramedullary nail also has drawbacks. In the case of nailing for forearm fracture, the interlocking screw needs to be fixed during the procedure. Therefore, an additional incision must be made to insert the interlocking screw, and skin irritation may occur with the interlocking screw. Also, there is a possibility that nerve damage may occur while inserting the interlocking screw. For proximal ulna shaft fractures, the length and thickness of the intramedullary nails are standardized, so they do not fit or should be cut out for Asians, and sometimes require prebending into a serpentine shape [18,19]. Since the diameter is also standardized, if friction between the intramedullary nail and the cortical bone does not occur, it may cause the movement of the bone fragments deteriorating stability [20]. Moreover, there is more radiation exposure due to C-arm in the operation than plate osteosynthesis [16], and after surgery, it is necessary to use immobilization with a brace or splint until bridging callus occurs in X-ray [10].
Keeping these things in mind, we considered a surgical method that does not have large skin incision like plate osteosynthesis and may not use additional interlocking screws like intramedullary nail. The author has previously published a paper and a technical note on HCS and pinning techniques for metacarpal bone fracture and ulna head and neck fracture [21,22]. Wadsworth [23] reported a 100% union in six patients using a partially threaded intramedullary screw in an olecranon fracture or osteotomy, and a full ROM was observed at 1-year follow-up. Johnson et al. [24] also reported that full motion was possible in a group of 28 patients, and Hong et al. [25] published a case report showing good results with intramedullary screw fixation in a proximal ulna fracture with a dorsal wound. With this in mind, we have a question whether surgery is possible using HCS and Steinmann pins, so we have verified the experiment measuring bending strength by using sawbone.
In our results, Steinmann pin was the strongest and plate osteosynthesis was the weakest. Regarding the plate, breakage of the plate did not occur, and pull-out fracture of the sawbone was observed (Fig. 3A). This is thought to have occurred because the plate was short and the sawbone was weaker than the actual bone. The strongest measured force of the Steinmann pin is thought due to the fact that the diameter of the Steinmann pin is longer than the HCS. However, as the bending goes on, the movement of the pin was checked and as there is no thread, it is considered to be weak in terms of pulling strength and rotation strength. When the strength of the sawbone is considered to be that of the osteoporotic bone, it can be applied by increasing the length of the plate, but in this case, the incision length increases. For these reasons, although HCS seems to have greater anatomical stability compared to Steinmann pin due to thread, both fixation methods can be sufficient alternative methods and also be better for patients with osteoporosis with minimized incision and less skin irritation [26,27].
As a limitation of this study, sawbone has the advantage of providing a uniform specimen, but does not reflect failure occurring at the fixative and bone interface because the physical properties are different from the actual cortical bone. Also, the number of experimental groups was small. As in the reference thesis using sawbone, 10 attempts were made [28], but due to the problem of research expenses, only seven groups were available. However, we tried to secure statistical significance with more numbers than six groups of reference papers using cadaver [29]. Of course, as expected, plate osteosynthesis would be excellent in rotation and axial force, but the study was conducted as the first trial for alternative method for plate. Also, unlike distal, the proximal ulna shaft is affected most by bending force rather than rotation and axial. Therefore, only bending force was performed as an initial study along with the reason for limiting the research cost. A study comparing rotation and axial force should also be conducted later. The cyclic load of proximal ulna identified in the reference was 30 to 300 N [28], which was much lower than the force performed in this study, so no studies on repetitive and cyclic loading were conducted. Moreover, it was not possible to compare the union rate later.
Fig. 2.
(A) ElectroPuls E3000; Instron, Norwood, MA, USA. (B) Three-point bending test; span distance, 80 mm.

Fig. 3.
Post experimental gross photos of sawbone fixed with each method. (A) Fixed with plate and screws. (B) Fixed with headless compression screw. (C) Fixed with Steinmann pins.

Table 1.
Bending strength results of three fixation groups
Table 2.
Comparison of bending strengths of three fixation groups
| Group | Bending strength (N) | p-value |
|---|---|---|
| Plate and screws (a) | 521.7 (339.5–675.8) | <0.001 (b>c>a) |
| Steinmann pins (b) | 812.6 (794.0–832.7) | |
| HCS (c) | 706.4 (662.9–725.2) |
Table 3.
Results of the post-hoc test for evaluating significant differences among the fixation groups
| Group | p-valuea) |
|---|---|
| Plate and screws vs. Steinmann pins | <0.001 |
| Plate and screws vs. HCS | 0.064 |
| Steinmann pins vs. HCS | 0.047 |
REFERENCES
2. Sarmiento A, Latta LL, Zych G, McKeever P, Zagorski JP. Isolated ulnar shaft fractures treated with functional braces. J Orthop Trauma. 1998;12:420-4.


3. Corea JR, Brakenbury PH, Blakemore ME. The treatment of isolated fractures of the ulnar shaft in adults. Injury. 1981;12:365-70.


4. Brakenbury PH, Corea JR, Blakemore ME. Non-union of the isolated fracture of the ulnar shaft in adults. Injury. 1981;12:371-5.


5. Anderson LD, Sisk D, Tooms RE, Park WI 3rd. Compression-plate fixation in acute diaphyseal fractures of the radius and ulna. J Bone Joint Surg Am. 1975;57:287-97.


6. Chapman MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute fractures of the diaphyses of the radius and ulna. J Bone Joint Surg Am. 1989;71:159-69.


7. Hadden WA, Reschauer R, Seggl W. Results of AO plate fixation of forearm shaft fractures in adults. Injury. 1983;15:44-52.


8. Müller ME, Allgöwer M, Willenegger H. Technique of internal fixation of fractures. NewYork: Springer; 1965.


9. Saikia K, Bhuyan S, Bhattacharya T, Borgohain M, Jitesh P, Ahmed F. Internal fixation of fractures of both bones forearm: comparison of locked compression and limited contact dynamic compression plate. Indian J Orthop. 2011;45:417-21.
10. Lee YH, Lee SK, Chung MS, Baek GH, Gong HS, Kim KH. Interlocking contoured intramedullary nail fixation for selected diaphyseal fractures of the forearm in adults. J Bone Joint Surg Am. 2008;90:1891-8.


11. Moss JP, Bynum DK. Diaphyseal fractures of the radius and ulna in adults. Hand Clin. 2007;23:143-51.


12. Droll KP, Perna P, Potter J, Harniman E, Schemitsch EH, McKee MD. Outcomes following plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 2007;89:2619-24.


13. Kim SB, Heo YM, Yi JW, Lee JB, Lim BG. Shaft fractures of both forearm bones: the outcomes of surgical treatment with plating only and combined plating and intramedullary nailing. Clin Orthop Surg. 2015;7:282-90.



14.
Sixto R Jr
Kortenbach JA
Avuthu S
Wich M
Sanders R
Steinmann S
. DePuy Products, Inc, assignee. Fracture fixation plate for the olecranon of the proximal ulna patent. United States patent US8182517B2. 2012 May 22.
15. Siebenlist S, Buchholz A, Braun KF. Fractures of the proximal ulna: current concepts in surgical management. EFORT Open Rev. 2019;4:1-9.



16. Ozkaya U, Kiliç A, Ozdoğan U, Beng K, Kabukçuoğlu Y. Comparison between locked intramedullary nailing and plate osteosynthesis in the management of adult forearm fractures. Acta Orthop Traumatol Turc. 2009;43:14-20.


17. Rand JA, An KN, Chao EY, Kelly PJ. A comparison of the effect of open intramedullary nailing and compression-plate fixation on fracture-site blood flow and fracture union. J Bone Joint Surg Am. 1981;63:427-42.


18. Gao H, Luo CF, Zhang CQ, Shi HP, Fan CY, Zen BF. Internal fixation of diaphyseal fractures of the forearm by interlocking intramedullary nail: short-term results in eighteen patients. J Orthop Trauma. 2005;19:384-91.


19. Weckbach A, Blattert TR, Weisser Ch. Interlocking nailing of forearm fractures. Arch Orthop Trauma Surg. 2006;126:309-15.



20. Lee S, Lee HS, Sung YB, Yum JK. Interlocking intramedullary nailing of forearm shaft fractures in adults. J Korean Fract Soc. 2009;22:30-8.


21. Oh JR, Kim DS, Yeom JS, Kang SK, Kim YT. A comparative study of tensile strength of three operative fixation techniques for metacarpal shaft fractures in adults: a cadaver study. Clin Orthop Surg. 2019;11:120-5.



22. Oh JR, Park J. Intramedullary stabilization technique using headless compression screws for distal ulnar fractures. Clin Orthop Surg. 2020;12:130-4.



23. Wadsworth TG. Screw fixation of the olecranon after fracture or osteotomy. Clin Orthop Relat Res. 1976;(119):197-201.

24. Johnson RP, Roetker A, Schwab JP. Olecranon fractures treated with AO screw and tension bands. Orthopedics. 1986;9:66-8.


25. Hong CC, Han F, Decruz J, Pannirselvam V, Murphy D. Intramedullary compression device for proximal ulna fracture. Singapore Med J. 2015;56:e17-20.



26. DeKeyser GJ, Kellam PJ, Haller JM. Locked plating and advanced augmentation techniques in osteoporotic fractures. Orthop Clin North Am. 2019;50:159-69.


27. Cornell CN. Internal fracture fixation in patients with osteoporosis. J Am Acad Orthop Surg. 2003;11:109-19.


28. Hopf JC, Nowak TE, Mehler D, Arand C, Gruszka D, Rommens PM. Nailing of proximal ulna fractures: biomechanical comparison of a new locked nail with angular stable plating. Eur J Trauma Emerg Surg. 2019 Nov 1 [Epub]. https://doi.org/10.1007/s00068-019-01254-7.